Facts A squint is a condition where your eyes look in different directions. One eye turns inwards, outwards, upwards or downwards while the other eye looks forwards. The medical name for a squint is strabismus. The misalignment of the eyes can be caused by different factors. It can be an early developmental problem where the… Continue reading Paediatric Strabismus
Myopia
Myopia is a common refractive condition which causes individuals to be near-sighted: they see near objects clearly but distant objects are blurry. Myopia occurs when the cornea and lens focus the light in front of the retina instead of exactly on it. Symptoms of myopia include; difficulty seeing distant objects, squinting frequently, holding books or… Continue reading Myopia
Lacrimal Probing in Children
The tear duct is a channel/passage which runs from a tiny opening in the medial lids through the bone to the inside of the nose, and drains the tears and mucus the eye produces. It should open just before or just after birth but sometimes remains blocked for a considerable time after that, causing watering… Continue reading Lacrimal Probing in Children
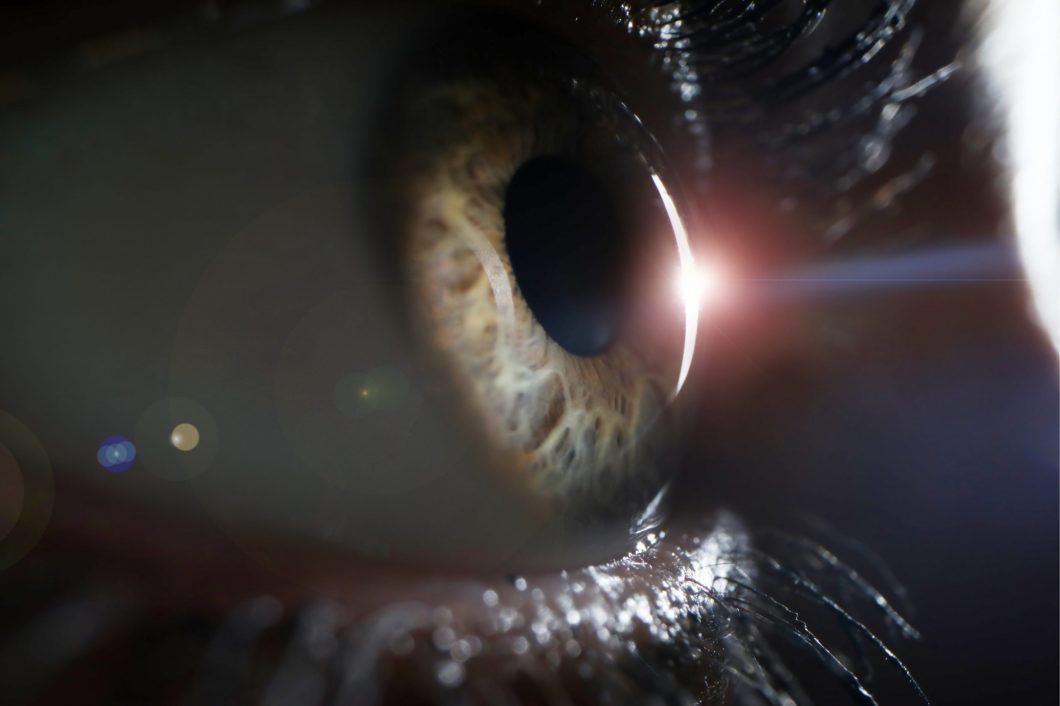
Keratoconus
Keratoconus is a progressive thinning of the cornea. The cornea is the clear front window of the eye, which, along with the intra-ocular lens, focuses light on to the retina. The cornea normally is a smooth, round dome-shaped structure; however in keratoconus it becomes very thin and irregular and it starts to protrude from the… Continue reading Keratoconus
Intravitreal Injection
The macula is the central part of the retina at the back of the eye. It is responsible for fine vision (reading, writing, watching television, and recognising faces). Patients with diabetes may develop macular oedema (swelling of the retina) due to leaking of fluid from blood vessels. This causes the vision to become blurred. A… Continue reading Intravitreal Injection
Hypermetropia
A refractive condition of the eye in which vision is better for distant objects than for near objects. It can be called far sightedness or hypermetropia. Symptoms of Hypermetropia can include; blurred vision, asthenopia (eye strain), accommodative dysfunction, binocular dysfunction, amblyopia and strabismus. It results from the eyeball being smaller than average, causing images to… Continue reading Hypermetropia
High Precision Refractive Surgery
When you decide on an eye laser treatment, you expect the best possible results. The more fully developed the methods are, the better the outcome will be. The SCHWIND AMARIS 750S offers you the leading technology for your laser treatment – superior in all important aspects: Speed, precision, safety and comfort.
Diabetic Retinopathy
Introduction Diabetic retinopathy is a complication of diabetes and leads to high blood sugar, resulting in retinal disease, which can interfere with its ability to transmit images to the brain through the optic nerve. Blood vessels in the retina play an important role in supplying it with oxygen and nutrients, which keep it healthy and… Continue reading Diabetic Retinopathy
Corneal Transplantation (PK)
Why do you need a corneal transplant? The cornea is a window of transparent tissue at the front of the eyeball. It allows light to pass into the eye and provides focus so that images can be seen. Various diseases or injury can make the cornea either cloudy or out of shape. This prevents the… Continue reading Corneal Transplantation (PK)
Corneal Transplantation (EK)
Why do you need a corneal transplant? The cornea is a window of transparent tissue at the front of the eyeball. It allows light to pass into the eye and provides focus so that images can be seen. Various diseases or injury can make the cornea either cloudy or out of shape. This prevents the normal passage of light and… Continue reading Corneal Transplantation (EK)
Corneal Transplantation (DALK)
Why do you need a corneal transplant? The cornea is a window of transparent tissue at the front of the eyeball. It allows light to pass into the eye and provides focus so that images can be seen. Various diseases or injury can make the cornea either cloudy or out of shape. This prevents the… Continue reading Corneal Transplantation (DALK)
Cataract Surgery Treatment
Facts The term cataract derives from the view we get when looking through a waterfall. A cataract is the clouding or opacity of the lens inside the eye. The lens has the shape of a lentil and lies behind the coloured part of the eye, the iris. In a normal eye, this lens is clear.… Continue reading Cataract Surgery Treatment