MBBch, FRCSEd Consultant Ophthalmologist Specialist in Cataract, Cornea and Refractive Vision Correction Surgery GCAA Approved Specialist Aeromedical Medical Examiner Associate Professor of Ophthalmology (Adjunct) Dr Osama Giledi is a highly experienced consultant ophthalmologist who specialises in Cornea, Anterior Segment, Cataract and Refractive Surgery. He is also skilled in managing ocular surface problems including severe dry… Continue reading Dr. Osama Giledi
Dr. Osama Giledi
MBBch, FRCSEd Consultant Ophthalmologist Specialist in Cataract, Cornea and Refractive Vision Correction Surgery GCAA Approved Specialist Aeromedical Medical Examiner Associate Professor of Ophthalmology (Adjunct) Dr Osama Giledi is a highly experienced consultant ophthalmologist who specialises in Cornea, Anterior Segment, Cataract and Refractive Surgery. He is also skilled in managing ocular surface problems including severe dry… Continue reading Dr. Osama Giledi
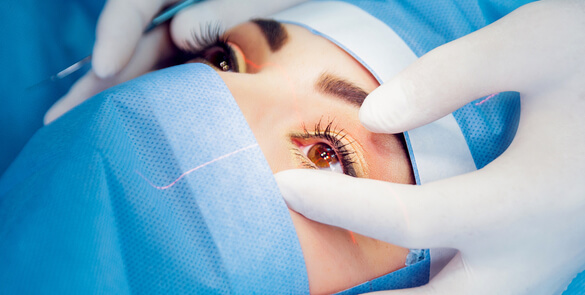
Information about Cyclodiode Laser Treatment
The diode laser is a highly concentrated beam of light, which can be used to target and treat a selected area. Sometimes, laser treatment is recommended in order to avoid or delay the need for more invasive surgery. The diode laser is used to produce very small burns in the ciliary body, which produces the… Continue reading Information about Cyclodiode Laser Treatment
Vitrectomy Surgery
A vitrectomy surgery is microsurgery performed to remove the jelly and replace it by a saline solution, gas or a special type of silicone oil. The most common reasons for operating on the retina are retinal detachment, diabetes and scarring on the retina. For more information about vitrectomy surgery in Dubai, contact us today.
Trabeculectomy
The operation to control the pressure within your eye is called a Trabeculectomy (trab-ec-u-lec-tomy). A Trabeculectomy operationis recommended for patients whose glaucoma continues to progress despite using eye drops and/or having laser treatment.The goal of the Trabeculectomy surgery is to help lower and control the eye pressure. The eye pressure is known as intraocular pressure.… Continue reading Trabeculectomy
Squint Surgery In Children
This information aims to answer some of the questions you may have about squint surgery. The information does not cover everything as every patient and squint is different. Your surgeon will discuss your particular case with you. Please ask the clinical staff about anything you want to be made clear. What are the aims of… Continue reading Squint Surgery In Children
Squint Surgery in Adults
This information aims to answer some of the questions you may have about squint surgery. However, it does not cover everything as every patient and squint is different. Your surgeon will discuss your particular case with you. Please ask the clinical staff about anything you want to be made clear. What is the aim of… Continue reading Squint Surgery in Adults
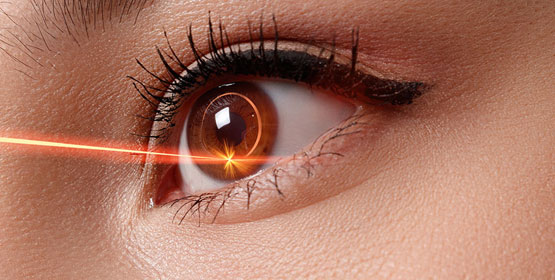
Selective Laser Trabeculoplasty
Selective Laser Trabeculoplasty (SLT) is a procedure used to reduce the pressure in the eye (also known as intra-ocular pressure). A laser beam is applied to the drainage channels, which helps to unclog them. This means the aqeous humour flows through the channels better, reducing the pressure in the eye. This is not a permanent… Continue reading Selective Laser Trabeculoplasty
Refractive Surgery
Most refractive errors can be corrected (or at least improved) by means of Refractive Surgery. This is a generic term, which comprises both Laser Refractive Surgery and correction by means of lens implants inside the eye. The latter is called Phakic intraocular lens (IOL) surgery. Most refractive errors can be corrected (or at least improved)… Continue reading Refractive Surgery
Presbyopia
Presbyopia is a vision condition which makes it difficult to focus on close objects. During middle age, usually beginning in the 40s, people experience blurred vision at near points, such as when reading, sewing or working at the computer. Presbyopia is a natural part of the ageing process of the eye. It is not a… Continue reading Presbyopia
Posterior Vitreous Detachment
PVD is a common degenerative change, which affects one or both eyes in many people after middle age. It may present earlier in shortsighted patients or those who have sustained traumas to the eyes. Thickening of the jelly casts shadows on the retina and are seen as floating shapes. These black “floaters”in your vision move… Continue reading Posterior Vitreous Detachment
Post-Operative Instructions
Following Retinal Surgery on leaving the hospital you are advised to have a quiet evening at home and to avoid strenuous exercise. For General Anaesthetic patients, as above and: Do not drive a vehicle Do not make any crucial financial decision Do not eat heavy meals or drink alcohol for 24 hours after being discharged