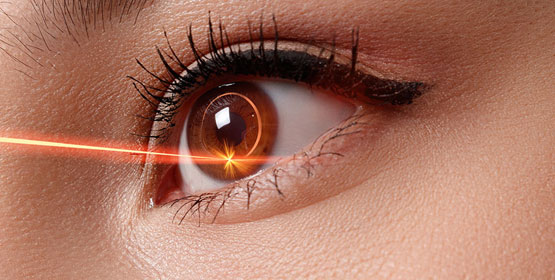
Most refractive errors can be corrected (or at least improved) by means of Refractive Surgery. This is a generic term, which comprises both Laser Refractive Surgery and correction by means of lens implants inside the eye. The latter is called Phakic intraocular lens (IOL) surgery. Most refractive errors can be corrected (or at least improved)… Continue reading Refractive Surgery
Presbyopia
Presbyopia is a vision condition which makes it difficult to focus on close objects. During middle age, usually beginning in the 40s, people experience blurred vision at near points, such as when reading, sewing or working at the computer. Presbyopia is a natural part of the ageing process of the eye. It is not a… Continue reading Presbyopia
Posterior Vitreous Detachment
PVD is a common degenerative change, which affects one or both eyes in many people after middle age. It may present earlier in shortsighted patients or those who have sustained traumas to the eyes. Thickening of the jelly casts shadows on the retina and are seen as floating shapes. These black “floaters”in your vision move… Continue reading Posterior Vitreous Detachment
Post-Operative Instructions
Following Retinal Surgery on leaving the hospital you are advised to have a quiet evening at home and to avoid strenuous exercise. For General Anaesthetic patients, as above and: Do not drive a vehicle Do not make any crucial financial decision Do not eat heavy meals or drink alcohol for 24 hours after being discharged
Myopia
Myopia is a common refractive condition which causes individuals to be near-sighted: they see near objects clearly but distant objects are blurry. Myopia occurs when the cornea and lens focus the light in front of the retina instead of exactly on it. Symptoms of myopia include; difficulty seeing distant objects, squinting frequently, holding books or… Continue reading Myopia
Corneal Transplantation (PK)
Why do you need a corneal transplant? The cornea is a window of transparent tissue at the front of the eyeball. It allows light to pass into the eye and provides focus so that images can be seen. Various diseases or injury can make the cornea either cloudy or out of shape. This prevents the… Continue reading Corneal Transplantation (PK)
Corneal Transplantation (EK)
Why do you need a corneal transplant? The cornea is a window of transparent tissue at the front of the eyeball. It allows light to pass into the eye and provides focus so that images can be seen. Various diseases or injury can make the cornea either cloudy or out of shape. This prevents the normal passage of light and… Continue reading Corneal Transplantation (EK)
Corneal Transplantation (DALK)
Why do you need a corneal transplant? The cornea is a window of transparent tissue at the front of the eyeball. It allows light to pass into the eye and provides focus so that images can be seen. Various diseases or injury can make the cornea either cloudy or out of shape. This prevents the… Continue reading Corneal Transplantation (DALK)