Why do you need a corneal transplant?
The cornea is a window of transparent tissue at the front of the eyeball. It allows light to pass into the eye and provides focus so that images can be seen clearly. Various diseases or injury can make the cornea either cloudy or change shape. This prevents the normal passage of light into the eye and affects vision.
The cornea has 5 layers (two outer and inner thin layers and a thick middle layer)
Types of Corneal Transplants:
- Deep Anterior Lamellar Keratoplasty (DALK)
- Superficial Anterior Lamellar Keratoplasty (SALK)
- Endothelial Keratoplasty ( DSAEK and DMEK)
- Penetrating Keratoplasty
DALK removes the outer three layers of the cornea and replaces them with donor layers to give a partial-thickness corneal transplant. 90% of patients achieve driving standard of vision but glasses or lenses may be needed or even another surgery; full recovery may take up to 18 months. There are risks with DALK but serious complications are rare. Rejection of the transplanted cornea can also occur but in less than 10% of cases in the 2 years after surgery and it is easy to treat as the rejection does not affect the rear corneal layer (endothelium). DALK generally has a lower risk. However, DALK has a slightly lower chance of achieving 6/6 vision (excellent vision) than with full thickness grafts.
Endothelial Keratoplasty (EK) replaces the inside layer of the cornea with a donor layer inserted through a small incision without the need to suture the graft. Most patients achieve driving vision, sometimes with glasses, and it can take up to 6 months to see the full benefits. It is a new type of corneal graft and complications are less serious, these include rejection of the transplanted cornea, graft failure, glaucoma and graft dislocation, which may require the repositioning of the graft by using air, which can be done easily under topical anesthesia. EK offers faster recovery compared to full-thickness grafts, due to the smaller incision and no suture related problems such as astigmatism, broken suture or inflammation.
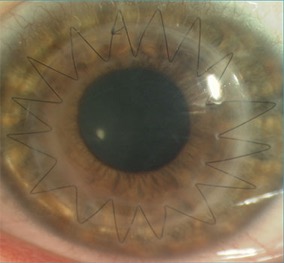
Penetrating Keratoplasty is a full thickness transplant and 75% of patients achieve driving vision, possibly needing vision aids or another surgery, and around 18 months for full improvement of vision. Risks are rare but can be serious and sight threatening including corneal transplant rejection, graft failure, glaucoma, cataract.
All the corneal transplant operations are performed under general or local anaesthetic and take about one hour. Patients are examined after surgery and generally go home the same day. They need to use steroid drops for about 1 year, or less for Endothelium Keratoplasty.
Understanding red eye – the symptoms, causes, and red eye treatment
What is red eye?
A bloodshot ‘red eye’ may be worrying but is rarely serious or causes pain.
Symptoms often disappear within a few days, without treatment.
But if it does not improve within a few days, there may be a more serious problem.
Symptoms of red eye
You will need to see an eye specialist for a diagnosis and red eye treatment, if you have:
- painful red eye
- other symptoms including reduced vision, sensitivity to light, or a severe headache and sickness
- recently had any injury to the eye – especially a blow with a sharp object
Common causes of red eye With a painless red eye, the most likely causes are conjunctivitis or a burst blood vessel, which don’t usually affect the vision.
Conjunctivitis Conjunctivitis is inflammation of the conjunctiva, which is the thin layer of tissue covering the eyeball and inner surfaces of the eyelids.
The inflammation causes the blood vessels on the eye to become swollen, and a bloodshot look, along with a gritty feel.
There can be other symptoms with conjunctivitis – such as itchy eyes or watery eyes.
An eye specialist may recommend:
- regularly clean away any crusting or discharge around the eye
- temporarily stop using contact lenses until the eye is better
- washing your hands regularly and avoiding sharing pillows/towels to help prevent the spread of infection
- using antibiotic eye drops for bacterial infections of the eye or medications for allergies such as pollen
Burst blood vessel in the eye A burst blood vessel on the eye surface can cause a bright red blotch called a subconjunctival haemorrhage. It can look alarming, but it’s not usually serious and should clear up on its own within a few weeks.
What causes painful red eye? There are several possible reasons and they can be serious.
Iritis is inflammation of the iris (coloured part of the eye) – symptoms include red eye but there may be other symptoms such as sensitivity to light, blurred vision, or a headache. Red eye treatment with steroid medication reduces the inflammation. Iritis rarely leads to any severe problems but see an eye specialist.
Acute glaucoma
If your red eye is severe and painful, with nausea and seeing halos around lights, and your vision is blurred or cloudy, this may be acute glaucoma – a serious condition with a sudden increase in eye pressure and you must see an eye specialist immediately.
Corneal ulcer (ulcer on the cornea)
An ulcer on the cornea (the clear outer layer at the front of the eyeball) can cause the eye to become red and sensitive to light, with discomfort in your eye. Bacterial corneal ulcers are usually seen in people who wear contact lenses. Your ophthalmologist will advise on red eye treatment.
A scratch to the cornea or particle in the eye
A particle in the eye can also cause a painful red eye. The best option is to go to an accident and emergency department.
Enucleation operation is necessary to treat eye cancer whereas Evisceration operation is necessary to treat an eye when it has been damaged through an accident. An enucleation operation is where the eye ball is removed. Evisceration operation is where the inside contents of the eye are removed, leaving the outer shell and the muscles intact. Both operations and orbital implant might be used to enhance orbital volume. After surgery, a temporary transparent plastic shell is put in the eye socket to allow healing and give it shape.
The plastic shell is then replaced with a prosthesis (artificial eye) which is shaped in the form of a large-size contact lens and covers the implanted orbit in the socket of the eye. Instructions on how to remove and clean the artificial eye should be provided.
Complications
Complications are rare but all operations carry some risk and complications such as bleeding, infections and swelling can sometimes occur after surgery. Beyond the operation, irritation of the eye socket, discharge or the ball implant becoming exposed are complications that can affect patients longer term.
Before the operation
Patients are admitted to hospital the day before the operation, to allow time for a variety of tests, including blood, x-rays of the chest and scans. The operation is carried out under general anaesthetic. Once healing of the eye socket is complete, an artificial eye can be fitted on a temporary basis.
Cleaning and maintaining the eye socket, artificial eye and the shell is important and the nursing team will provide instructions on all aspects before the patient goes home. Once outside the hospital patients can keep the eye uncovered to allow faster healing; if the swelling of the eye is a concern, then a pair of sunglasses can be worn.
The shell can sometimes fall out but this is very rare and if it does happen, then the shell should be cleaned carefully, following the hospital’s instructions.
Your artificial eye
It takes about one month to make a permanent artificial eye and in the interim period, a temporary prosthesis is fitted. The permanent artificial eye will give a broad range of movement of the eye.
Patients can live a normal life with an artificial eye, including sleeping with it in place, once the eye socket has healed. This includes wearing make-up, swimming and water sports, although goggles should be worn to make sure the artificial eye cannot fall out and be lost.
After the operation
After surgery, the eye is covered and dressed which is kept in place for a day following the operation.
Uveitis is inflammation inside the eye and affects women, men and children. Though relatively uncommon, it can be serious with complications that can cause loss of vision. It is estimated that the more serious types of uveitis are responsible for 1 in every 10 cases of visual impairment. This means that early diagnosis and treatment is critical.
Symptoms of uveitis:
Symptoms of Uveitis can include a painful red eye that ranges from mild aching to intense discomfort; blurred or cloudy vision; sensitivity to light; new ‘floaters’ on the eye; loss vision; and headaches. The symptoms can develop suddenly or appear gradually over days and can last for a short time, or be more prolonged or recurring.
- a painful red eye – ranging from mild aching to intense discomfort; the eye can feel tender or bruised
- In children, the eye may not become red
- blurred or cloudy vision
- sensitivity to light
- marked or new floaters – shadows, webs, dots or veils that move across the field of vision
- loss of the ability to see objects at the side of your field of vision
- a pupil shaped differently or that doesn’t get smaller when reacting to light
- headaches
Types of uveitis
- anterior uveitis is the most common type of uveitis – three out of four cases, causing pain and redness and may recur,
- intermediate uveitis – inflammation can cause floaters and blurred vision
- posterior uveitis – inflammation at the back of the eye can cause problems with vision
Causes:
The causes of Uveitis remain unclear but often involve a malfunction of the body’s immune system, infections or injury to the eye, including after eye surgery. In half of the cases, a cause or systemic disease is found, but in the other half no cause can be identified..
Treatment
Eye drops are often used for uveitis affecting the front of the eye, and injections, tablets and capsules are usually used to treat uveitis in the middle and back of the eye.
The initial treatment is steroid medication (corticosteroids). Other treatment options include ant-inflammatory medication, immunosuppressive agents, biologic drugs and even surgery.
Treatment is often done in conjunction with another medical specialist like a rheumatologist.
Uveitis can be:
- acute – when it resolves quickly after treatment
- recurrent – when repeated episodes are separated by gaps of several months
- chronic – when the condition continues long-term or requires long-term medication to control it
Complications
Most cases respond quickly to treatment but there is a risk of complications like cataract, glaucoma loss of vision, and permanent visual damage.
The retina is a thin layer of tissue that lines the back of the inside of the eye, located near the optic nerve.
The role of the retina is to change the light focused on to it by the eye’s lens into a signal that the brain can then ‘see’ as a visual image.
Thanks to the retina, we can recognise colours and we can see different intensity of light – light and shade. This means we can carry out all out our basic daily tasks such as reading and driving.
The mechanism by which we see involves the teamwork of the retina capturing the light through its photoreceptor cells, together with the optic nerve which conveys the information through the optic nerve at the back of the eye to the brain. We then rely on the brain to tell us what the image really is, so we can understand it.
If something interrupts this visual process, such as damage to the retina, it may lead to vision loss and even blindness.
Because of the retina’s vital role in vision, any damage to it can cause permanent blindness.
Retinal conditions
Damage to the retina is one of the most serious eye conditions and detachment of the retina can be especially threatening, and may stop the retina from processing light. This results in an urgent medical emergency.
This process prevents the brain from receiving this information, and so causes blindness.
Conditions at the back of the eye are treated medically using drugs, eye drops or lasers.
These conditions include age-related macular degeneration (AMD), retinitis pigmentosa, diabetic retinopathy, retinal blood vessel blockages and inflammation at the back of the eye (uveitis).
- Macular degeneration – deterioration of the central vision
- Diabetic eye disease
- Retinal detachment – where the retina detaches from the back of the eye
- Retinoblastoma – cancer of the retina, which is most common in young children.
- Macular pucker – where the macula has scar tissue
- Macular hole – a small break in the macula that usually happens to people over the age of 60
- Floaters – cobwebs or specks in your field of vision
Some of these diseases are chronic – slow, long term conditions – and others are acute – sudden, serious deterioration and may be localised or can affect just the macula or the entire retina.
Age-related Macular Degeneration is the most common and affects older people. Hereditary forms of the disease with an early onset also exist, such as Stargardts, Best’s Disease or progressive Cone Dystrophy. Generally, these diseases cause severe visual impairment but rarely result in complete blindness.
In contrast, hereditary retinal degenerations that attack the whole of the retina are usually more severe.
Examples of these conditions include Usher Syndrome and Retinitis Pigmentosa (RP), both of which are common types of these diseases.
First symptoms may include loss of the outside of the field of vision (leading to ‘tunnel vision’) and problems with night vision;
People with Ushers Syndrome suffer from congenital deafness or severe loss of hearing.
People who are suffering from Retina and looking for more information on it can contact a retina specialist in Dubai at Moorfields Eye Hospital.
What does it mean when your eyes are itchy?
Usually, itchy eyes are the result of an allergy although there are other possible causes, depending on the symptoms.
What are the causes?
Itchy eyes are generally caused by an allergy – such as pollen, dust or animal dander. – that triggers a reaction in the body and the release of histamines in the tissues around the eyes, which results in itching, red eyes and swollen eyes.
Eye allergies can be seasonal or perennial.
All sorts of products and their ingredients may give you itchy eyes and these include solutions you use for your contact lenses, some kinds of eye makeup and skins creams, lotions and soaps; even eye drops for dry eyes can cause the itching.
You may have other symptoms along with the itching, such as burning eyes and these could be caused by a gland dysfunction or dry eye syndrome, rather than any allergies.
Blepharitis is a condition that makes your eyelids red and swollen; it’s usually caused by bacteria but microscopic mites are another possible cause.
Treatment
Artificial tears and eye drops to stop any allergy can be used to treat itchy eyes.
Sometimes, relief from the symptoms of itchy eyes can only be relieved by using oral medicines or even prescription eye drops.
The treatments that address the real cause of the itchy eyes – such as dry eye or a seasonal allergy – and not just the symptoms are the most effective.
Consult your eye doctor to determine the most effective remedy for itchy eyes and most suitable for your particular needs.
The cures for itchy eyes can include drops for allergies or even artificial tears, antibiotics or other medications.
The most important basic advice to anyone with itchy eyes is not to rub them because it just makes them worse and even more itchy. You could even create more problems by scratching the cornea or causing an eye infection through bacteria on your fingers.
Eye allergies
Eye allergies are also known as ‘allergic conjunctivitis’.
Contact conjunctivitis is when cosmetic products or other ingredients are the cause of the eye problems.
An allergy to contact lenses is called giant papillary conjunctivitis.
Treating Eye Allergies
Interestingly, medicines used for other allergies may also give you some relief for itchy eyes and other eye allergies.
When you need immediate relief from the irritating symptoms of itchy eyes, then tablets or drops can help.
If you’re still having symptoms, your doctor may suggest allergy injections to expose you to increasing amounts of an allergen over time and allow your body to get used to it gradually.
Other Ways to Reduce Symptoms
- Don’t forget to wear sunglasses when outside in sunlight because they can also block some of the pollen and other irritants from getting into your eyes.
- Rinse your eyes with water or apply a cold, wet washcloth.
- You can use artificial tears to wash and moisten dry eyes and these will also help remove anything in the eyes that may irritate them.
- Take out your contact lenses.
There are around 250,000 blepharoplasty procedures done every year, making it the most common cosmetic surgery done on the eyelids, in the world
But the results of the surgery can differ very broadly from one patient to the next.
An important part of the preparation is an analysis by the surgeon of the ageing process of the patient, so that the surgery can produce the best cosmetic results.
Lacrymal surgery
Problems concerning the tear channels and the lachrymal ducts such as a ‘watery eye’ can be treated by surgery. The aim is to restore the normal flow of tears down to the nose when a blockage has occurred.
Orbital problems
These are related to the bony sockets of the eyes and their nerves, muscles, arteries, veins, fat and lachrymal glands.
Aesthetic Oculoplastics
A Oculoplastic Surgeon also performs aesthetic non surgical treatments and surgery to eyelids such as dermal fillers and botulinum toxin injections.
Blepharoplasty (eyelid surgery)
Blepharoplasty surgery is possible whilst the patient is under local or general anaesthetic .
An upper blepharoplasty may take about one hour to complete, whilst surgery on the lower lid may take up to two hours.
Most patients usually go home the same day of the surgery.
You should take about a week off work to recover from eyelid surgery. You won’t be able to drive for a few days after the operation.
The surgeon should explain possible side effects and complications, and how they would be treated if they occurred. Sometimes, patients find the desired cosmetic effect wasn’t achieved and feel they need another operation.
Choosing your cosmetic surgeon
Before you have cosmetic surgery you will need to choose a surgeon who has the appropriate training, skills and experience to carry out the procedure.
The surgeon should know about the results you want and why, and you should talk about the options and possible results of surgery.
It is reassuring for the surgeon to explain clearly what happens during surgery and a good question to ask is about the possible complications of surgery and which are the most common, in the surgeon’s experience.
Moorfields Eye Hospital Dubai provides refractive laser eye surgery with all the latest techniques and is a referral centre for complications.
Refraction
When the focusing power of the eye does not allow you to see clearly, there is a refractive error.
Laser surgery, or laser refractive surgery is quick and life changing.
Common conditions treated by laser eye surgery
Short- or near-sightedness (Myopia)
This is where near objects can be seen clearly but distant ones are blurred.
Long- or far-sightedness (Hypermetropia/Hyperopia)
This is where distant objects are seen more clearly than near ones.
Presbyopia
Presbyopia is the normal decline in focusing power as we age and is not altered by laser refractive surgery.
Astigmatism
Astigmatism is usually the result of the cornea being misshapen.
Your initial assessment
The initial assessment is to confirm there are no reasons not to do surgery.
Excimer Laser refractive Surgery
Laser eye surgery is used for short-sightedness (myopia), astigmatism, and long-sightedness (hyperopia),
Types of laser eye surgery
PRK (photorefractive keratectomy)
PRK is mainly used for correcting low prescriptions with a healing process lasting several months. The surgeon needs to remove the outer layer of the cornea (called the epithelial layers) mechanically or Alcohol-assisted.
LASEK (laser epithelial keratomileusis)
LASEK is similar to PRK but with fewer complications and faster healing.
IntraLase and LASIK
LASIK (laser in situ keratomileusis) is a common procedure to correct long-sightedness and short-sightedness with minimal pain and fast recovery.
WaveFront Optimized
Wavefront-guided LASIK is a tailor-made form of LASIK that provides better results in most cases.
EpiLASIK EpiLASIK
EpiLASIK EpiLASIK is a new procedure using an epikeratome that creates a thin flap of epithelium.
Yag Laser Eye Surgery
Be informed
Patients should –
- Have a very clear understanding of the procedure
- Know what outcomes to expect
- Choose a refractive laser eye surgeon.
What are the risks?
- Complications in less than 5% of cases
- Some people have a problem with dry eyes
- In rare cases, the shape of the eye may be unstable.
Am I a candidate?
Patients suitable for treatment –
- Age 21 years or over
- Stable prescription
- Healthy eyes
- Good general health
LASIK (laser in situ keratomileusis) is a common vision correction surgical procedure that reshapes the cornea and is used to treat patients with near-sightedness, short-sightedness, farsightedness and astigmatism.
The latest laser vision correction technology is now available in Dubai / UAE.
To make the right choice about refractive surgery, talk to your eye doctor – good results depend on careful evaluation of your eyes and a clear understanding of each procedure.
Lasik eye surgery has become routine at any age – for patients as young as 18 years old and up to 50 and even beyond.
How does Lasik work?
A local anaesthetic is applied using eye drops and a small flap is created in the top of the cornea, and the underlying tissue is shaped using a laser.
Advantages of LASIK eye surgery
- LASIK is effective -around 96% of patients get their desired vision
- LASIK procedure is associated with very little pain
- Vision is corrected almost immediately.
- No bandages or stitches are required.
- Adjustments can also be made even years after surgery to further correct vision if needed.
- After LASIK, almost all patients notice a dramatic reduction in the need for glasses or contact lenses and most patients don’t need them at all.
Disadvantages of LASIK eye surgery
- LASIK is one of the safest eye surgeries although it is a technically complex procedure and problems may occur, although they are rare.
- LASIK can cause a reduction in ’best’ vision – although this is also rare.
Are there any potential side effects
- Some patients experience some discomfort in 24 to 48 hours after surgery.
- Other side effects, although rare, may include Glare, Seeing halos around images, Difficulty driving at night, Fluctuating vision, Dry eyes
Is LASIK surgery right for you?
LASIK surgery suits people with:
- Near-sightedness (myopia), in which you see nearby objects clearly
- Farsightedness (hyperopia), in which you see far objects clearly
- Astigmatism, which causes general blurred vision.
Most older adults lose the ability to focus on nearby objects (presbyopia) and wear two glasses or varifoccal glasses. LASIK can improve their distance vision, but a patient might still need to wear near vision glasses only.
Blurred vision is one of the most common eye problems amongst patients and very often leads patients to ask for advice.
Blurred vision is caused by a wide range of eye conditions and can be a symptom of a number of serious and not-so-serious eye problems.
Of course, vision changes with age and blurred vision – especially affecting near vision – occurs due to the normal process of ageing.
Relatively harmless temporary conditions such as dry eye can be a cause, for example, but there are others.
Potential causes of blurred vision
Symptoms of Cataract often start with blurring of night-time vision which then may start to affect daytime vision as well.
Glaucoma can present in its later stages with some vision loss; early symptoms are a reduction of the peripheral vision. Acute glaucoma presents with a sudden and painful reduction of vision.
Retinopathy which is often caused by diabetes leads to blurred vision because of swelling or bleeding in the retina; this is a serious condition that can lead to blindness if left untreated.
Likewise, macular degeneration results in the loss of light-detecting neurones at the back of the eye and leads to blurred vision, distortion or loss of central vision and fading of colour vision. Usually, these symptoms affect patients over the age of 60 and are often most noticeable when focusing on a task such as reading.
Much rarer causes for blurred vision include haemorrhagic or thrombotic stroke, TIA (transient ischemic attack), and malignant hypertension, occlusions of the central retinal blood vessels, brain tumours, temporal arteritis or thyroid disorders.
Treatment for blurred vision
Treatment of the vision problem depends on the cause and an examination by an ophthalmologist is recommended.
Depending on the diagnosis, treatments could include steroid eye drops may be prescribed taking care to ensure that no damage is possible through their use.
The simple rule is that any acute, painful eye condition with blurred vision or actual vision loss should be treated as an emergency and medical advice and treatment should be undertaken immediately.
Some of the main causes of visual impairment today include:
Cataracts
Cataracts cloud the lens of the eye blocking light and resulting in a loss of vision clarity. They are very common and cause about 50% of blindness in the world, affecting 20 million people. The good news is that they are preventable and treatable.
Diabetic Retinopathy
Diabetes if uncontrolled can lead to serious health complications including diabetic retinopathy, which can result in blindness, as high blood sugar damages the retina.
Diabetic retinopathy is one of the main causes of blindness but this can be avoided with early diagnosis and treatment.
Diabetic maculopathy
Diabetic maculopathy is the result of damage to the macula which is the part of the eye which gives us our central vision and can be caused by retinopathy.
Diabetic macular oedema (DMO) is a common problem and leads to a build up of fluid on the macular resulting in damage.
Glaucoma
Glaucoma can result in damage to the optic nerve, connecting the brain to the eye, and is a very common eye condition – affecting around 80 million people around the world. It can lead to loss of vision if not detected and treated in the early stages. Glaucoma usually develops because the fluid in the eye cannot drain properly, increasing the pressure inside the eye and applying pressure to the optic nerve.
Vision loss starts at the periphery of the field of vision and people may struggle to see well in low light.
Age-related Macular Degeneration (AMD).
For people aged 60 and above, AMD is a common form of the loss of central vision caused by damage to the macula, which sits at the rear of eye.
Retinitis Pigmentosa (RP)
Retinitis Pigmentosa is a genetic eye disease inherited from generation to generation and is a serious condition that gradually leads to vision and night vision loss and even total blindness. It can start in childhood or adolescence.
Corneal blindness
Corneal Blindness is a visual impairment that develops through the clouding of the cornea, scarring or some other infection that affects the transparency of cornea, leading to permanent blindness and comprises a range of eye disease, infection and injury that damage the corneal tissues.
Eye infections can invade the eyeball or the area around it – they are generally microorganisms that can be harmful, including viruses, bacteria and fungi.
Causes and Types of Eye Infections
Conjunctivitis is a common infection usually caused by bacteria or virus; it’s very contagious and often affects children in schools or other places where it is easily passed from child to child. It gives the eye a pink tinge, which is why it is also known as ‘pink eye’.
There are other types of infections caused by viruses (viral keratitis), such as ocular herpes caused by the herpes simplex virus.
Fungal eye infections (fungal keratitis) can be caused by a penetrating injury allowing the fungus to invade the area.
People who wear contact lenses are vulnerable to infections caused by parasites (acanthamoeba keratitis) which can be serious and even threaten sight. Contact lens users generally need to take special precautions and ensure lenses are well cared for and cleaned properly.
The trachoma infection is very common in some areas of the developing world where it may also be one of the main causes of blindness. It can be spread by flies and one of the main problems with this is reinfection and so proper hygiene and access to treatment is essential.
Endophthalmitis is a bacterial infection that affects the inside of the eye (because of an injury or very rarely after eye surgery) and can cause blindness without immediate powerful antibiotic treatment. There is also a type of mould that can cause the problem, although this is rare.
Mould that penetrates the eye’s interior also can cause endophthalmitis, though rarely.
A stye of chalazion is an infection that affects the inside of the eyelids.
Dacryocystitis is an infection of the tear ducts that inflames and blocks the system that drains tears from the eyes.
Corneal ulcers can be caused by an infection and may be connected to the use of contact lenses; these are serious infections and can result in very severe loss of vision if they are not treated.
There are some infections – such as endophthalmitis – that go deeper into the inside areas of the eye and they can be sight-threatening.
Orbital cellulitis may attack the soft tissue around the eyelids and this infection is a serious emergency and needs treatment to stop it spreading.
Eye Infection Treatments
With early diagnosis and treatment, most of the common bacterial infections will resolve themselves with the use of prescribed medications such as antibiotics – eye drops, ointments and compresses.
Most viral infections disappear with little effort but if they are severe, antiviral drops may be needed to reduce inflammation.
How to Prevent Eye Infections
Good hygiene and especially hand washing is essential before touching any area of the eye and when using contact lenses.