This blog on Intraocular lenses (IOLs) was authored by Dr. Salman Waqar, Consultant Ophthalmologist in Cataract and Glaucoma Surgery.
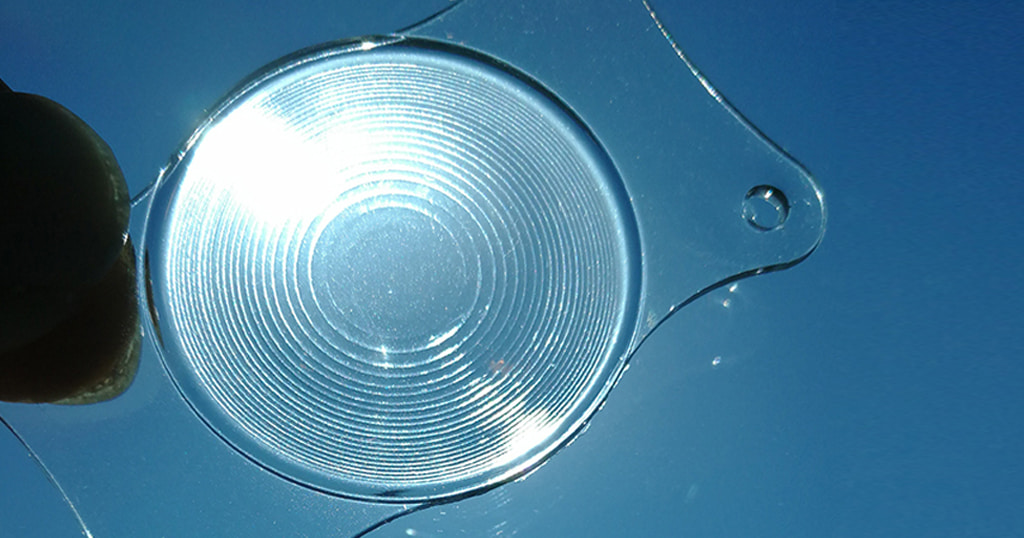
IOLs (intraocular lenses) are implanted into a patient’s eye during surgery to remove cataracts. During the ‘refractive lens exchange’ procedure, the surgeon replaces the natural lens with these medical devices.
Before the 1980s and the introduction of intraocular lenses, patients who had cataracts removed had to wear very thick eyeglasses or special contact lenses to see after surgery; no medical device was available to implant in the eye to replace the focusing power of the natural lens.
Today, there is a wide variety of premium IOLs to choose from. The most suitable intraocular lens for a patient depends on many factors, including lifestyle and specific visual needs. There are ‘premium’ multifocal intraocular lenses available with advanced features beyond those found in basic single-vision IOLs.
During your preoperative examination and consultation, Dr Sohaib Mustafa can help you choose the best IOL for your needs.
Toric IOLs
The choice of IOLs includes the option of a type of lens called Toric Multifocal IOLs. These premium lenses can also correct a range of vision issues, including near/farsightedness and astigmatism. This is made possible because they contain a range of power across the lens, and the surgeon can align the lens to the patient’s cornea and correct the astigmatism very accurately during surgery.
Multifocal IOLs
Multifocal IOLs are another category of presbyopia-correcting IOLs that can decrease your need for glasses for reading or computer use after cataract surgery.
Like multifocal contact lenses, these premium IOLs have added magnification in different parts of the lens to expand your range of vision so you can see objects clearly at all distances without glasses or contact lenses. Some studies have shown multifocal IOLs tend to provide better near vision than IOLs, but they also are more likely to cause glare or mildly blurred distance vision as a tradeoff.
Dr. Mustafa can help you decide whether you are a good candidate for multifocal IOLs during your preoperative examination and consultation.
Monovision
An alternative to multifocal IOLs for correcting presbyopia is monovision, which is not an IOL.
This is the technique of fully correcting the vision in one eye and intentionally making the other eye mildly nearsighted. In this situation, the fully corrected eye sees distant objects clearly (but glasses are needed to see objects nearby), and the mildly nearsighted eye sees close objects very well without glasses (but distant objects are not so clear). This allows the patient to adapt, and to use the dominant eye for distance and the non-dominant eye for near vision. However, this option does not suit everyone. If it is considered, the patient would need a contact lens trial to simulate this combination of vision correction (although this would not be a perfect trial if there is a cataract) to allow the patient to decide whether it would be tolerable before proceeding with surgery.
This week’s blog on Refractive Errors has been contributed by Dr Osama Giledi, Consultant Ophthalmologist, Specialist in Cataract, Cornea and Refractive Vision Correction Surgery
Refractive Errors
In a normal eye, the light (the image that we see) will focus onto the retina, and the quality of this image depends on the balance between the length of the eye, corneal power and eye lens power; any change in the balance of these three factors will create a refractive error, which needs correcting.
- Myopia (nearsightedness): In an eye with Myopia, the image focuses in front of the retina and the vision is blurred, mainly when viewing objects over distance.
- Hypermetropia / Hyperopia (farsightedness): The image focuses behind the retina and the vision can be blurred, especially for objects close by.
- Astigmatism: Astigmatism occurs when the cornea is shaped more like a rugby ball than a football. If astigmatism is significant, images reaching the retina are stretched and distorted as it does not have one single point of focus and the vision is blurred, both for objects that are near or distant.
- Presbyopia: Experiencing difficulties when reading, especially over the age of 40, is called Presbyopia and this is a completely natural (and unavoidable) phenomenon. It happens because the eye gradually loses its ability to focus on objects that are nearby, as the crystalline lens becomes stiffer. This process starts at around the age of 40-45 and is normally completed by the age of 65.
Figure 1: Eye model showing the cornea (A), the iris and the pupil (B), the crystalline lens (C), the retina (D). The most common refractive errors such as myopia (M) and hypermetropia (H) are shown compared to the normal (emmetropic) eye (E) where the images form exactly on the retina.
Refractive Surgery
Most refractive errors can be corrected (or at least improved) by Refractive Surgery. This is a generic term, which comprises both Laser Refractive Surgery on the Cornea, correction by implanted lenses inside the eye called Phakic intraocular lens (IOL) surgery, or the replacement of the natural lens (either a clear lens or one with cataract ) with an intraocular implant – usually a multifocal implant to improve distance , intermediate and near vision.
Laser Refractive Surgery
We can change the shape of the cornea to correct the refractive error. In a case of myopia, the surgeon uses the laser to remove a circle of central corneal tissue to flatten the cornea, which then focuses the image onto the retina.
When the myopia is very high or when the cornea is too thin, laser may not be considered a safe option because the tissue removed may result in a weaker cornea (and a risk of developing keratoconus). In these cases, Phakic IOL surgery is a very good alternative treatment, provided that your eyes are suitable.
To treat hypermetropia, the surgeon uses the laser to change the shape of the central cornea to increase the focusing power of the eye.
To treat astigmatism, the laser removes tissue in an elliptical pattern transforming a rugby ball shaped cornea to a round football shape.
Types of Laser Refractive Surgery:
Laser refractive surgery can be divided into two broad categories: LASIK and SURFACE ABLATIONS.
In LASIK, a flap is lifted and the main laser reshaping is carried out under the flap whereas in SURFACE ABLATIONS, the reshaping is done directly on the corneal surface.
In LASIK, the vision recovers quickly and typically you should be able to resume your work and drive within 1-2 days. There may also be a mild discomfort lasting only for a few hours after surgery.
In SURFACE ABLATIONS, the epithelium (the outermost layer of the cornea which regenerates spontaneously every few days) is removed using different techniques (PRK, LASEK, Epi-LASIK, Trans-PRK). This is like creating a scratch on the eye surface but in a controlled manner. Then the laser excimer (exactly the same laser used for LASIK) reshapes the stroma, the underlying layer.
Surface ablations are initially more uncomfortable for the first two days compared to LASIK, and there is also a slower visual recovery which can take about five days but this procedure is ideal for patients with thin corneas or dry eyes and in those patients whose occupation or hobbies make it more dangerous to create a flap.
We use the latest method called Trans-PRK in which the epithelium is entirely removed by the laser and the eye is not touched by the surgeon. Trans-PRK tends to have a shorter recovery time and less discomfort than other surface laser methods (PRK, LASEK, Epi-LASIK).
Phakic Intraocular Lens (IOL) Surgery
Phakic lOLs are designed for people with high degrees of myopia that cannot be safely corrected by laser refractive surgery. These ‘Implantable contact lenses’ called Visian ICLs are implanted inside the eye in front of the crystalline lens and behind the iris. It is a very effective, safe and reliable procedure for suitable candidates.
This week’s blog on Advanced Diabetic Retinopathy has been contributed by Dr. Ammar Safar, Chief Medical Officer, Consultant Ophthalmologist and Vitreoretinal Surgeon.
Advanced Diabetic Retinopathy
The effects of uncontrolled diabetes (through diet or medications) on the eye can be devastating in several ways.
The most severe effect is on the Retina, a sensitive membrane that lines the inside of the eye and creates the images that we see. In this blog, I will address some of the common and important questions people have about the impact of advanced diabetes on the eye, also known as Advanced Diabetic Retinopathy:
Can diabetes make me go completely blind?
Yes. Neglected and uncontrolled diabetes can lead to the complete loss of vision through one of three mechanisms:
- Bleeding inside the eye, which becomes completely filled with blood instead of clear liquid.
- The build-up of scar tissue on the retina, which then pulls on the retina and causes it to separate from the wall of the eye, a condition called Traction Retinal Detachment.
- Complete collapse of the normal retinal blood vessels, which leads to the death of the cells that generate the vision due to a lack of oxygen and nutrients (Retinal ischemia).
A combination of the three mechanisms is possible but the last mechanism is relatively rare.
Can vision loss due to advanced diabetes be treated?
Fortunately, yes! The advances in this area of medicine over the past decade or so have resulted in remarkable breakthroughs. In our (Moorfields?) experience, over 92% of the acute vision loss caused by the effects of the complications of advanced diabetes on the retina can now be reversed and vision can be restored.
A surgical procedure called ‘Pars Plana Vitrectomy’ can be performed to stop the bleeding in the eye and remove any possible scar tissue that can be pulling the retina. This allows restoration of vision. The procedure is performed under local anesthesia with no stiches and no need for an overnight hospital stay. New medical treatments are currently being investigated that would reverse the collapse of retinal vessels and hopefully prevent any retinal cell death.
My blood sugar level is well controlled but I am still having retinal problems. Why?
Diabetes is a very malicious disease. For years and sometimes decades, there may be no symptoms at all. Most people discover they have type 2 diabetes during a routine blood test and a regular health check up, without any complaints about symptoms.
Unfortunately, if the blood sugar level is uncontrolled over several years, damage is slowly taking place all over the body including the retina of the eye. The problems and complications appear after several years of poor control and it is at this point that most people realize they need to take this disease very seriously. At this stage, controlling the sugar is crucial to stopping the damage but unfortunately control does not result in immediate effects on the vision. Rather, good control of blood sugar levels pays off after a few years of consistent management and compliance with treatment.
The best approach to dealing with the retinal complications of diabetes is to avoid them completely by performing routine yearly eye check-ups and adhering to a strict diet and medical regimen, but the reality is that we react to how we feel. We are very fortunate to live in an era where even severe vision loss caused by the complications of diabetes can be reversed and functional vision can be restored.
Age-Related Macular Degeneration
Age-Related Macular Degeneration (AMD) is one of the most common causes of the loss of vision in people aged 50 and older. Worldwide, the number of people with age-related macular degeneration is projected to reach 196 million by 2020, increasing to 288 million by 2040. (1)
The vision loss occurs due to damage to the central part of the retina, or macula, which is the most sensitive part of the retina and enables us to have sharp and detailed vision when we look straight ahead. When the macula is damaged, the centre of our field of vision may appear blurred, distorted, or dark. This loss of central vision, even without leading to complete blindness, can still however interfere with everyday tasks such as reading, writing, driving or recognising faces.
The progression rate of the disease varies and when it is in the initial stages, any vision-related symptoms may develop slowly. However, there are cases in which the progression of the disease is rapid and loss of vision may be sudden.
The most significant risk factor for AMD is age but research has shown that smoking doubles the risk of AMD. Furthermore, AMD is more common among certain groups within the community and genetics are relevant because people with a family history of AMD are at higher risk, and more than 20 genes have now been identified as affecting the risk of developing AMD (source nei.nih.gov).
In the early and intermediate stages, AMD can typically be detected only with a comprehensive examination of the retina, often using dilating drops to provide a better view of the back of the eye. The examination normally includes the measurement of visual acuity, visualisation of the retina with a slit lamp and ancillary tests such as OCT and Fluorescein & Indocyanine Green Angiography (FFA & ICGA).
Early AMD;
the disease is characterised by the presence of medium-sized drusen (yellow deposits beneath the retina). People with early AMD typically do not have vision loss.
Initially there may be no symptoms but over time the quality of the vision deteriorates. The sharpness of vision may be lost and colours may appear washed out and lack definition. Glare is another symptom that may be experienced.
Intermediate AMD;
in these cases, drusen are larger and often joined together and may be associated with pigment changes in the retina. At this stage there may be some vision loss, but most people will not experience any symptoms.
Late AMD;
in addition to drusen, people with late AMD have vision loss caused by damage to the macula. There are two types of late AMD:
1: Geographic Atrophy (also called dry AMD) in which the progressive damage from drusen ultimately leads to cell death and loss of vision
2: Neovascular AMD (also called wet AMD) in which abnormal blood vessels grow underneath or through the retina. These vessels can leak fluid and blood, which accumulates in the retina leading to swelling and damage of the macula. The damage may be very quick and severe.
It is possible to have both geographic atrophy and neovascular AMD in the same eye, and either type can appear first.
Whilst there is no specific treatment for early AMD, research has found that daily intake of certain high-dose vitamins and minerals can slow progression of the disease in people who have intermediate AMD, and in those who have late AMD in one eye only. The first AREDS trial showed that a combination of vitamin C, vitamin E, beta-carotene, zinc, and copper can reduce the risk of late AMD by 25 percent.
With neovascular AMD, abnormally high levels of vascular endothelial growth factor (VEGF) are secreted in the eyes – VEGF is a protein that promotes the growth of new abnormal blood vessels. Anti-VEGF injection therapy blocks this growth and therefore slows the progression of the disease.
Today, most neovascular AMD is treated with intravitreal injections, with laser being reserved for a selected minority of cases. Typically, multiple monthly injections are required and the earlier treatment starts, the higher the chances of better vision results.
AMD has few symptoms in the early stages, so it is important to have your eyes examined regularly. If you are at risk of AMD because of age, family history, lifestyle, or some combination of these factors, you should not wait for changes in your vision before being checked for AMD.
If you have late AMD in one eye only, you may not notice any changes in your overall vision. With the other eye seeing clearly, you may still be able to drive, read, and see fine details. However, having late AMD in one eye means you are at increased risk of late AMD in your other eye.
1 Wong, WL Lancet Glob Health. 2014 Feb;2(2):e106-16
2 nei.nih.gov
This week’s blog on Cataract has been contributed by Dr. Avinash Gurbaxani, Consultant Ophthalmic Surgeon in Uveitis and Medical Retinal Diseases and Cataract Surgery.
What is cataract?
Cataract is the clouding of the natural lens of the eye. This is generally a slow process related to age, in which the transparent lens gradually loses its transparency, making the vision cloudy or dull. Other factors such as Diabetes or eye surgery, or medications like corticosteroids, can also cause cataract.
What are the symptoms?
Initially there may be no symptoms but over time the quality of the vision deteriorates. The sharpness of vision may be lost and colours may appear washed out and lack definition. Glare is another symptom that may be experienced.
Does cataract threaten vision?
Having a cataract does not damage your eye and vision loss due to cataract is reversible. Patients with visual symptoms should be examined for cataract by an ophthalmologist.
What is the treatment?
Cataract is treated by surgery. This is one of the most frequently performed operations in the world and also one of the most successful. Modern day cataract surgery is very safe and effective. The cloudy lens is removed and an artificial lens is implanted. It takes 15-20 minutes and is painless, and is most often done under local anesthesia. The surgery is performed on a day patient basis.
Will I need glasses?
The eye is examined and an appropriate lens is implanted. Monofocal lenses usually correct distance vision and you may only need reading glasses. Multifocal lenses correct for distance and near vision and may eliminate the need for glasses. Based on the eye examination, the ophthalmologist can advise on which lens is most suitable for you.
How long does recovery take?
Recovery depends on the overall health of the eye and patients can return to regular activities the very next day. Full vision recovery may take a few days up to a month. There are no major lifestyle restrictions after the operation.
Selecting a pair of sunglasses
Sunglasses may help you look cool and fashionable but they are also designed to protect your eyes, so choosing a pair of sunglasses is about more than just looking good.
1) The lenses
UV protection
It’s important to protect against excessive exposure to ultraviolet (UV) rays.
Make sure that you check to see if they protect against 99% of UVA rays and at least 95% of UVB rays.
If they are labeled as ‘cosmetic’ or don’t provide any information about UV protection, it’s better not to get them.
Distortion
Make sure you check for distortion by holding the lenses up to a fluorescent lamp. As you move the sunglasses up and down, check that there is no wave distortion that will also distort your vision. If there is none, this is a good sign.
Scratch resistance
Finally, make sure that the lenses in the sunglasses are scratch resistant, as scratched sunglasses are damaged and useless.
The colour
Note that the colour of the lenses doesn’t just affect your fashion statement, it affects how well you detect contrast and differentiate colours. The colour of the lenses you choose can make a difference to your vision and can enhance contrast, which is always useful, but the colour of the lens can also affect the ability of the eye to detect colour differences, which may be a problem – when driving, for example.
2) The frame
Shape
Sunglasses come in all shapes and sizes. Generally, finding a contrast between the shape of your face and the shape of the frame will look good. For example, if you have a round face, more angular frames will work well, and if your face is squarer, a rounder softer frame shape will look good.
Fit
Like any pair of glasses, choose sunglasses that fit your face and are comfortable to wear, so take care when trying on new pairs. They should feel well balanced and not squeeze the head, ears or nose, and sit on the bridge of the nose without touching the eyelashes.
The sunglasses should balance on the bridge of the nose and ears; if they feel inclined to one side, you need to adjust them.
The size
Make sure that the lens area is not too small, so that it will be able to block sunlight effectively
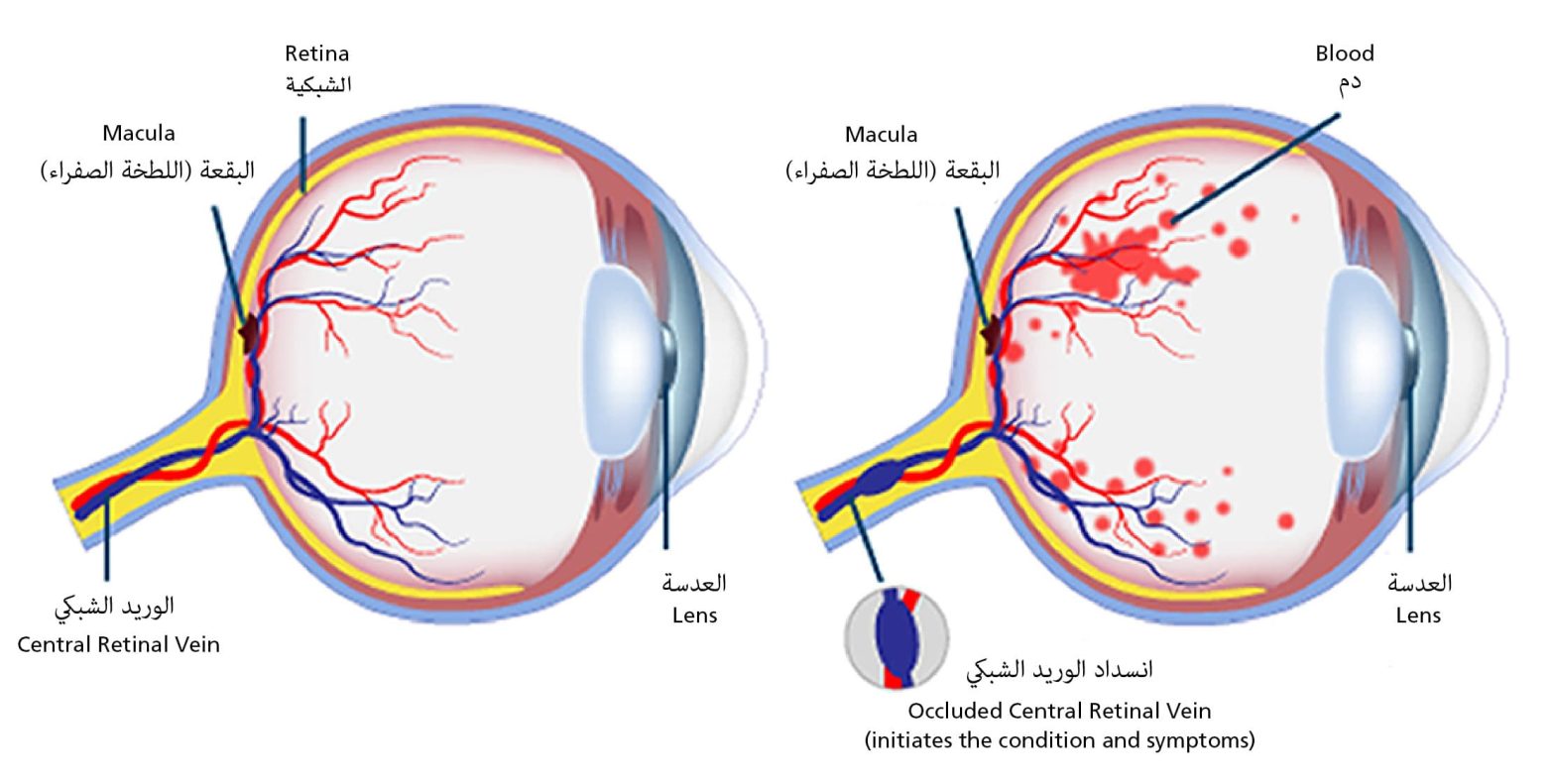
Retinal Vein Occlusion (RVO) is one of the most common vascular disorders affecting the retina. It is a leading cause of sudden, painless vision loss, particularly in adults over 50 years of age. Although the condition may sound alarming, early diagnosis and timely treatment can significantly improve outcomes and help preserve vision.
This guide is designed to help individuals and their families understand the causes of RVO, how it is diagnosed, and the available treatment options.
Retinal Vein Occlusion: What It Means & What to Do
Retinal Vein Occlusion occurs when one of the veins responsible for draining blood from the retina becomes blocked. The retina is the light-sensitive tissue located at the back of the eye, which is essential for processing visual information. When blood flow is interrupted, fluid may accumulate (known as macular oedema), leading to swelling, bleeding, and in severe cases, permanent vision loss.
This blockage usually affects one eye and can happen suddenly. The severity and treatment approach depend on the location and extent of the blockage.
Types of Retinal Vein Occlusion
There are two main types of Retinal Vein Occlusion, each with distinct characteristics:
- Central Retinal Vein Occlusion (CRVO): This occurs when the central vein responsible for draining the entire retina is blocked. CRVO is often associated with more significant vision impairment and may lead to complications such as macular oedema, abnormal blood vessel growth (neovascularisation), or increased eye pressure (neovascular glaucoma).
- Branch Retinal Vein Occlusion (BRVO): BRVO involves a blockage in one of the smaller branches of the central retinal vein. It tends to cause more localised and less severe vision loss compared to CRVO.
Causes Retinal Vein Occlusion
RVO is often linked to changes in blood vessels and underlying health conditions. Common risk factors include:
- Hypertension (high blood pressure): Chronic high blood pressure can damage the retinal vessels, increasing the risk of occlusion.
- Diabetes: Diabetes can lead to changes in blood vessels throughout the body, including those in the eye.
- Cardiovascular Disease: Conditions that affect circulation, such as atherosclerosis (hardening of the arteries), increase the risk of retinal vein blockage.
- Glaucoma: Elevated eye pressure can contribute to vein compression.
- Blood Clotting Disorders: Rare clotting conditions or thickened blood can contribute to blockages in the retina.
- High cholesterol (Hyperlipidaemia): Elevated lipid levels contribute to blood vessel narrowing and clot formation.
In some cases, RVO may occur without a known cause, particularly in younger individuals. This is why a comprehensive evaluation is essential.
Symptoms of Retinal Vein Occlusion
The most common symptom is a sudden, painless loss of vision in one eye. Other symptoms may include:
- Blurred or distorted central vision
- Partial or complete loss of vision in one eye
- Dark spots or floaters in the visual field
- A general dimming of vision
- Sudden onset of visual disturbances, such as dark patches or floaters
It is important to note that RVO is usually not associated with eye pain or redness, which distinguishes it from other acute eye conditions.
Diagnosing Retinal Vein Occlusion
Diagnosis is made during a comprehensive eye examination by an ophthalmologist. This may include:
- Dilated Fundus Examination: Using eye drops to dilate the pupil, the doctor examines the retina for signs of haemorrhage, swelling, or abnormal blood vessels.
- Optical Coherence Tomography (OCT): This non-invasive imaging test provides high-resolution images of the retina to detect macular swelling and monitor treatment response.
- Fluorescein Angiography: A special dye is used to identify areas of poor circulation or leakage from blood vessels.
- Visual acuity test and intraocular pressure (IOP) measurement: To assess baseline vision and rule out contributing factors, such as glaucoma.
These tests help differentiate between CRVO and BRVO, guiding the development of appropriate treatment plans.
Treatment options for Retinal Vein Occlusion
Although there is no direct way to unblock the vein, treatment focuses on reducing swelling, preserving vision, and managing the underlying causes.
Ocular treatments of Retinal Vein Occlusion
- Observation: In some cases, particularly with mild BRVO not affecting the central retina (macula), the eye may be monitored closely without immediate intervention
- Intravitreal Injections: These are the most common treatments for macular oedema resulting from RVO:
- Anti-VEGF (Vascular Endothelial Growth Factor) agents, such as ranibizumab or aflibercept, help reduce fluid buildup and prevent abnormal blood vessel growth.
- Steroid injections may be used if anti-VEGF is not effective or suitable.
Treatment is usually given over several months and personalised to each patient’s progress.
- Laser Photocoagulation: This may be used to treat areas of poor retinal circulation (non-perfusion) or to control abnormal blood vessel growth, especially in BRVO cases.
Systemic treatments of Retinal Vein Occlusion
Managing the underlying medical conditions is crucial in preventing further eye damage and reducing the risk of RVO recurrence. This includes:
- Controlling blood pressure
- Managing blood sugar levels in diabetic patients
- Treating high cholesterol
- Lifestyle changes such as quitting smoking, maintaining a healthy weight, and regular exercise
In some cases, your ophthalmologist may collaborate with a general physician or cardiologist for a coordinated care approach.
What Is the outlook for patients with RVO?
The visual outcome depends on several factors, including the location of the blockage, whether the macula is involved, and the timing of treatment initiation.
With appropriate care, many people regain stable or improved vision. However, long-term monitoring may be needed. If left untreated, complications such as neovascular glaucoma, retinal detachment, or persistent swelling can occur.
Living with Retinal Vein Occlusion
A diagnosis of RVO can feel overwhelming, but with support and proper management, many individuals adjust well. It is important to:
- Attend all follow-up appointments
- Adhere to medication schedules
- Monitor for any sudden changes in vision
- Take steps to maintain cardiovascular health
- Seek emotional support or low-vision rehabilitation if vision loss persists
When to see a Retina specialist in Dubai for Retinal Vein Occlusion?
If you experience sudden changes in your vision, especially in one eye, or have known risk factors such as diabetes or high blood pressure, it is essential to seek prompt medical care. Early diagnosis and treatment can be vision-saving.
At Moorfields Eye Hospital Dubai, our retina specialists provide expert care for all forms of Retinal Vein Occlusion, utilising advanced diagnostic imaging and evidence-based treatment plans tailored to each patient.
Frequently Asked Questions about Retinal Vein Occlusion
- Is Retinal Vein Occlusion the same as a stroke in the eye? While not technically the same, Retinal Vein Occlusion (RVO) is often referred to as an “eye stroke” because it involves a sudden blockage in one of the veins that drain blood from the retina, the light-sensitive tissue at the back of the eye. Much like a stroke in the brain, this blockage can disrupt normal function and lead to lasting damage. However, RVO occurs only in the eye and typically affects one side, whereas cerebral strokes involve brain tissue and may affect a wider range of functions.
- Can RVO cause total blindness? Complete blindness from RVO is rare; however, the condition can lead to significant vision impairment, especially if left untreated promptly. The most severe visual loss typically occurs when the macula, the part of the retina responsible for detailed central vision, is affected. Complications such as macular oedema or abnormal blood vessel growth (neovascularisation) can also contribute to vision loss. Timely diagnosis and ongoing treatment can help protect vision and prevent further deterioration.
- Is the condition painful? RVO is typically painless. Many patients only become aware of it after noticing a sudden change in vision, such as blurriness, dark spots, or partial loss of sight. The absence of pain can make early detection challenging, so it is important to seek immediate medical attention if you notice unexplained vision changes, even if there is no discomfort.
- Can I drive if I have RVO? Whether you can continue to drive depends on the degree of vision loss and its impact on your ability to see clearly, especially at night or in peripheral areas. Your ophthalmologist will assess your visual acuity and field of vision to determine if it is safe for you to drive. In some cases, restrictions may be advised for your safety and the safety of others.
- How can I prevent RVO from happening again? Prevention focuses on controlling the underlying risk factors that contribute to vein occlusion. This includes maintaining healthy blood pressure, managing diabetes and cholesterol levels, quitting smoking, and staying physically active. Regular follow-ups with both your ophthalmologist and primary care physician are vital.
- Will I need injections for the rest of my life? Not necessarily. Some patients respond well to a few initial injections and require less frequent treatments over time, while others may need long-term management to keep swelling under control. Your doctor will monitor your condition and adjust your treatment plan to suit your eye’s response and overall progress.
This week’s blog on Paediatric Cataract has been contributed by Dr Syed M. Asad Ali, Consultant Paediatric Ophthalmologist, Strabismus and Cataract Surgery
What is Cataract?
Cloudiness or opacity in the natural crystalline lens of the eye is called cataract. It is also called ‘white water’ or ‘white pearl’ because of its white appearance. Cataract is very common in people over the age of 50 but – contrary to common belief – it can happen at any age. When a child is born with a Cataract it’s called Congenital Cataract and it affects the vision by preventing all the light reaching the retina at the back of the eye.
Causes of Cataract in the young
Cataract can occur in one eye (unilateral) or both eyes (bilateral). In Western countries, the incidence of Cataract affecting childhood vision is about 3-4 cases in 10,000 live births. The incidence is higher in Asia.
Bilateral Cataracts can be caused by genetic mutations; over 15 gene defects have now been discovered. There are also systemic associations with metabolic disorders such as galactosemia, Wilson disease and diabetes. It has been noticed in people with Trisomy 21 (down syndrome) as well. If a mother acquires an infection such as rubella, herpes, toxoplasmosis or syphilis, this can cause Cataracts at birth.
Unilateral Cataracts are sometimes associated with other eye diseases like small eye, abnormal front of the eye (anterior segment dysgenesis), inflammation, vitreous and retinal diseases.
Any significant trauma (impact with a sharp or blunt object) to the eye can cause Cataract.
Presentation
At a very early age, parents may notice a white area at the centre of the pupil or an abnormal reflection in the pupil. Some children develop squint due to lazy eye caused by Unilateral Cataract. Children are sometimes brought to the ophthalmologist after failing a school eye test. In the case of Unilateral Cataract, even older children may not realise that they are only seeing with one eye, as they are able to manage well.
Treatment
Treatment of Cataracts depends on a number of factors like age at diagnosis, presence of Unilateral or Bilateral, mild or dense cataract and the presence of lazy eye. Dense Bilateral Cataracts at birth are operated on at around 6-8 weeks of age because early surgery can pose a high risk of Glaucoma (blue water) and delaying surgery beyond 3 months of age can limit the vision improvement, due to the development of lazy eyes. Unilateral Dense Cataract at birth has a poor visual prognosis because of the early development of lazy eye.
Mild Cataracts do occur but significant Cataract treatment involves surgery and the removal of the Cataract. In children under 3-4 years of age, Cataract removal also removes the part of front jelly (vitreous) of the eye.
An intraocular lens (IOL) is usually implanted in children above 1 year of age but this can be done earlier in unilateral cases. The power of the IOL selected also allows for the growth of the eye.
After surgery care is very important and may involve regular eye drops for 4-6 weeks after surgery, regular wearing of glasses, contact lenses and patching (covering the one eye with better vision) for the prescribed number of hours. This requires a lot of support and involvement of the parents
In these cases, early diagnosis and prompt treatment can save children from lifelong sight impairment.
It is important for all children to have regular eye check-ups.
This blog has been authored by Dr. Salman Waqar, Consultant Ophthalmologist in Cataract and Glaucoma Surgery for Children and Adults
While glaucoma is often associated with adults, it can also affect children, even from birth. Known as paediatric glaucoma or congenital glaucoma, this condition involves increased pressure inside the eye, which may damage the optic nerve and gradually affect a child’s side (peripheral) vision if not addressed early.
This blog outlines the causes, symptoms, diagnosis, and treatment options to help parents and caregivers understand the condition and seek timely care.
What Is Paediatric Glaucoma?
Paediatric glaucoma refers to a group of eye conditions in children where there is an abnormal increase in eye pressure. This happens when the fluid inside the eye, known as aqueous humour, does not drain properly through the eye’s natural drainage system.
In a healthy eye, this fluid flows in and out smoothly to maintain a stable pressure. In glaucoma, this balance is disrupted, leading to fluid build-up and increased pressure inside the eye. Over time, this pressure can damage the optic nerve that connects the eye to the brain.
Types of Paediatric Glaucoma
- Primary Congenital Glaucoma: The most common form, usually present at birth, caused by improper development of the eye’s drainage system during pregnancy. It affects around 1 in 10,000 births globally.
- Secondary Paediatric Glaucoma: This type may result from other eye conditions, previous eye surgery, trauma, or systemic conditions.
- Juvenile Open-Angle Glaucoma: Typically diagnosed in older children or teenagers, this type resembles adult glaucoma and also requires specialised care.
What are the causes of Glaucoma in children?
The cause of primary congenital glaucoma is often genetic and history of glaucoma in the family increases the risk. Other causes include:
- Improper development of the eye during pregnany
- Eye trauma or injury
- Past eye infections
- Inflammatory eye conditions
- Certain genetic syndromes such as Sturge-Weber, Axenfeld-Rieger)
What are the Symptoms of Glaucoma in children?
Young children cannot always describe what they see or feel. As a result, parents and caregivers must be vigilant for signs that could indicate a problem. Common symptoms include:
- Unusually large eyes: Increased pressure may cause the eyeball to stretch and appear abnormally large.
- Cloudy cornea: A hazy or milky-white appearance over the front of the eye.
- Excessive tearing: Frequent watery eyes without apparent cause
- Photophobia: Sensitivity to bright lights.
- Asymmetry between the eyes: A noticeable difference in eye size or shape between the two eyes.
If you notice any of these signs, it is important to seek care from a paediatric ophthalmologist or paediatric glaucoma specialist promptly.
How is Paediatric Glaucoma diagnosed?
Diagnosing glaucoma in infants and young children is complex and requires consultation with a specialised paediatric eye doctor. During the consultation with the specialist will utilise multiple techniques to ensure the correct diagnoses which include:
- Measuring the pressure inside the eye
- Checking the clarity of the cornea
- Using diagnostic imaging such as Optical Coherence Tomography (OCT) to assess the optic nerve
- Examining the drainage structures in and around the eyes
In young children who may not tolerate a full exam while awake, a specialised assessment under anaesthesia may be required. In certain cases, genetic testing may be recommended to identify inherited conditions.
Importance of early detection
Early detection can help preserve vision. Basic eye assessments during routine check-ups may include:
- Red reflex: A reddish glow that appears when light is shined into the eye. Its absence could indicate a problem with the cornea or lens.
- Corneal clarity: A cloudy cornea may point to elevated intraocular pressure.
These initial tests may not confirm glaucoma but can signal the need for further specialist evaluation.
What are the treatment options for glaucoma in children?
Treatment for paediatric glaucoma focuses on lowering the eye pressure to prevent further damage to the optic nerve. The appropriate treatment plan is tailored depending on the child’s age, glaucoma type, and severity
1. Medication: Eye drops or oral medicines to reduce fluid production or help fluid drain more effectively. Medications are often a temporary solution or used in preparation for surgery.
2. Surgery: Surgery is often the main approach for treatment of congenital glaucoma. Common procedures include:
- Goniotomy: A procedure that opens the drainage canals using a fine surgical tool.
- Trabeculotomy: A procedure used to create a new drainage pathway for fluids.
- Tube implants: These are surgically inserted devices to create a pathway for fluids inside the eye, used in complex or advanced cases.
The success of surgery depends heavily on early intervention, the child’s overall health, and regular follow-up. Like all surgeries, these procedures carry potential risks, which is why ongoing care is essential.
What happens after glaucoma treatment?
Children diagnosed with glaucoma require regular follow-up, even if the pressure is successfully managed. After surgery or medical treatment, ongoing care may involve:
- Eye pressure checks
- Monitoring optic nerve health
- Prescription glasses or contact lenses
- Visual aids if vision is affected
- Classroom and home support strategies
- Referral to low vision rehabilitation services if necessary
With early care and consistent monitoring, many children go on to lead full, independent lives. Adjustments such as bright lighting, the use of magnifiers, or support at school may be helpful.
Conclusion
Although rare, Paediatric Glaucoma is a serious condition that can affect a child’s vision if not managed early. However, when identified early and managed by a specialist, many children retain useful vision and enjoy a high quality of life.
If you have concerns about your child’s eye health or a family history of glaucoma, it is highly recommended to consult with a paediatric ophthalmologist or a paediatric glaucoma specialist in Dubai.
At Moorfields Eye Hospital Dubai, our glaucoma specialists are experts in diagnosing and caring for children with glaucoma. As a hospital accredited by JCI and ACHSI, we provide expert care in a warm, child-friendly environment, using the latest diagnostic technologies to ensure accurate and timely treatment
Frequently Asked Questions about Paediatric Glaucoma
- Is paediatric glaucoma hereditary?
Yes, certain forms of paediatric glaucoma are hereditary. In primary congenital glaucoma, which is the most common type seen in infants, genetics can play a significant role. If one or both parents have a history of glaucoma or other eye conditions, their child may have a higher risk of developing the condition. Additionally, some genetic syndromes linked to eye development abnormalities may include glaucoma as part of their presentation. If there is any family history of eye disease, it is important to inform your child’s ophthalmologist early on so that a tailored screening plan can be created. Genetic counselling may also be offered in some cases to assess risk for future children. - Can paediatric glaucoma affect both eyes?
Yes, paediatric glaucoma can affect both eyes, a condition referred to as bilateral glaucoma. In congenital cases, it is quite common for both eyes to be involved, although the degree of severity may vary from one eye to the other. This is why a thorough assessment of both eyes is essential, even if only one eye appears affected. Managing bilateral glaucoma may involve more complex treatment strategies, but with the proper care and follow-up, many children achieve good outcomes in both eyes. - How is paediatric glaucoma diagnosed in babies or toddlers who cannot communicate? Specialised paediatric ophthalmologists use a combination of clinical signs, imaging, and examinations under anaesthesia to assess eye pressure, corneal clarity, and optic nerve health when a child is too young to cooperate.
- What is the long-term outlook for children diagnosed with glaucoma?
The long-term outlook depends on how early the condition is diagnosed and how effectively it is treated. With prompt surgical or medical intervention and consistent follow-up care, many children with glaucoma can maintain usable vision into adulthood. However, because glaucoma causes permanent damage to the optic nerve, ongoing monitoring is essential to detect any pressure changes or vision deterioration. Some children may need additional procedures or vision aids over time, but many go on to lead full, independent lives. - Can children with glaucoma live a normal life?
With effective treatment, many children with glaucoma grow up attending mainstream schools, participating in sports, and enjoying social activities. Depending on the extent of vision loss, some adjustments may be necessary, such as classroom seating arrangements or using magnifiers. Emotional support from family, teachers, and healthcare providers is important in helping children adapt and thrive despite the diagnosis. - Are there any lifestyle changes or home adjustments needed after diagnosis?
There are several ways to support a child living with glaucoma. Ensure lighting is bright and evenly distributed at home to reduce eye strain. For reading and schoolwork, magnifiers or large-print materials may help. Some children may need to avoid high-impact sports or activities with a risk of eye injury. Most importantly, maintaining a strict medication routine and attending regular follow-up appointments are key to protecting their vision over time. Working closely with your child’s ophthalmologist will help determine the best support strategies tailored to their specific needs. - Can my child go blind from glaucoma?
If left untreated, glaucoma can cause permanent vision loss. However, with early diagnosis and effective treatment, most children retain functional vision and lead active lives.
Traditionally, the aim of cataract surgery has been to give patients the quality of vision to ensure a normal lifestyle including distance vision activities such as driving and watching movies. For clear near vision after cataract surgery, patients would often still require glasses for reading.
Nowadays, candidates for cataract surgery have a wide range of options, including multifocal IOLs (Intraocular Lenses) that offer total vision correction.
If you need cataract surgery and want more freedom from spectacles after surgery, then multifocal intraocular lenses are an excellent option to increase your range of clear vision. In fact, many people who choose multifocal intraocular lenses are generally glasses-free or may only need reading glasses occasionally for reading small print, after cataract surgery.
Who are the best candidates for multifocal IOLs?
If you are considering having a multifocal IOL implant, it’s important to understand that they also have their limitations.
If you are in a job that needs you to have the best possible distance vision at all times, or excellent night vision – for example if you are a pilot or someone who does a lot of night driving – then you probably are not a good candidate for multifocal IOL implants and regular monofocal (single-focus) lenses would be a better choice and provide very good distance vision. This would mean that you would need reading glasses to see well, up close.
Another thing to keep in mind is that if you have an associated visual condition other than a cataract (such as diabetic retinopathy, glaucoma or age related macular degeneration), you would be more satisfied with the results using regular monofocal IOLs. This is because multifocal IOLs need good visual capability in both eyes for optimal results.
Other considerations
To get the best visual results with multifocal IOLs, the exact placement of the lens in the eye is very important.
So, a cataract surgeon may also recommend a laser cataract surgery procedure using a femtosecond laser to help ensure accurate positioning of the multifocal IOL and get the best possible results from the lens.
This blog has been contributed by Dr. Luisa Sastre, Consultant Ophthalmologist in Medical Retina and Cataract Surgery.
Diabetes is a significant public health issue across the Gulf region, including the UAE, Saudi Arabia and Kuwait. According to the international diabetes federation, approximately 20.7% of UAE adults are living with diabetes, equating to around 1.25 million adults, or 1 in 6 adults.
Diabetes is a chronic condition that affects how the body absorbs, stores, and utilises sugar from food. When this process is impaired, it leads to hyperglycemia, elevated blood sugar levels. Over time, consistently high blood sugar levels can damage blood vessels and nerves, leading to complications in multiple organs, including the eyes.
One of the most serious eye-related complications of diabetes is Diabetic Retinopathy. Despite its potential severity, it often develops gradually and without noticeable symptoms, making regular eye screenings essential for all individuals living with Diabetes.
In this blog, we explore the connection between Diabetes and vision, explaining the causes and progression of diabetic retinopathy, and provide insights into modern treatment options available.
What are the different types of diabetes?
There are two main types of Diabetes:
- Type 1 Diabetes is typically diagnosed in children or young adults. It is often referred to as “insulin-dependent” Diabetes and results from an autoimmune process where the pancreas produces little or no insulin.
- Type 2 Diabetes is the most common form and primarily affects adults over the age of 40, although it is increasingly seen in younger individuals. It is closely linked to obesity, sedentary lifestyles, and genetic predisposition.
What are the genetic factors of diabetes?
- If one parent has type 2 Diabetes, the child’s risk is approximately 40%.
- If both parents are affected, the risk increases to 70%.
- For type 1 Diabetes, the hereditary risk is significantly lower at around 5%.
Diabetic Retinopathy: Causes, Risks & Treatment Options
Diabetic Retinopathy is a complication of diabetes that occurs when persistently high blood sugar levels damage the blood vessels of the retina which is the thin, light-sensitive tissue lining the back of the eye.
As the condition progresses, these vessels may swell, leak, or become blocked, resulting in reduced blood flow to the retina. In more advanced stages, abnormal new blood vessels may grow, potentially leading to bleeding, scar tissue formation, and further complications such as retinal detachment.
What leads to diabetic retinopathy?
There are various risk factors that contribute to the development of diabetic retinopathy, which include:
- Duration of diabetes (the longer a person has diabetes, the higher the risk)
- Poor blood sugar control
- High blood pressure
- Elevated cholesterol or lipid levels
- Kidney disease
- Pregnancy (in women with pre-existing diabetes)
What are the symptoms of diabetic retinopathy?
Diabetic Retinopathy often develops silently, without pain or obvious vision changes in the early stages. However, some individuals may experience:
- Blurred or fluctuating vision
- Impaired night vision
- Difficulty transitioning between light and dark
- Spots or dark strings (floaters) in their field of vision
- Partial or total vision loss in advanced cases
It is important to note that good vision does not rule out the presence of diabetic retinopathy. Regular diabetic eye examinations are important even in the absence of symptoms.
How is diabetic retinopathy diagnosed?
A retina specialist uses advanced diagnostic tools to detect and monitor diabetic retinopathy:
- Fundus Examination: A detailed evaluation of the retina using specialised lenses and lighting.
- Optical Coherence Tomography (OCT): A non-invasive imaging scan that captures cross-sectional views of the retina to detect swelling or structural changes.
- Fluorescein Angiography: A dye-based test used to assess blood vessel leakage and identify areas of poor circulation or abnormal growth.
These tests allow for accurate staging of the condition and guide the development of an individualised treatment plan.
What are the different stages of Diabetic Retinopathy?
- Mild Non-Proliferative Retinopathy: Small bulges in blood vessels (microaneurysms) appear.
- Moderate Non-Proliferative Retinopathy: Some blood vessels become blocked.
- Severe Non-Proliferative Retinopathy: More vessels are blocked, cutting off blood supply.
- Proliferative Diabetic Retinopathy (PDR): New, fragile blood vessels grow, which can bleed or cause scar tissue.
Another related condition, Diabetic Macular Oedema (DME), can occur at any stage and involves swelling in the central part of the retina (macula), resulting in blurred central vision.
Treatment Options for Diabetic Retinopathy
Treatment is tailored based on the severity and progression of the disease. Common options include:
- Observation: For early or mild cases, regular monitoring may be sufficient, especially if there are no symptoms or changes in vision.
- Intravitreal Injections: Medications such as anti-VEGF agents or steroids are injected directly into the eye to reduce retinal swelling, stop blood vessel leakage, and prevent new abnormal vessels from growing
- Laser Therapy
- Conventional Laser Photocoagulation: Targets leaking blood vessels or oxygen-deprived retinal areas in severe cases.
- Subthreshold Micropulse Laser: A gentler, more targeted approach that minimises damage to surrounding tissue.
- Subthreshold Micropulse Laser: A gentler, more targeted approach that minimises damage to surrounding tissue.
- Vitrectomy Surgery: In advanced cases involving retinal detachment, dense bleeding (vitreous haemorrhage), or scar tissue, surgery may be necessary to restore vision and prevent further damage.
Importance of early diagnosis for Diabetic Retinopathy
Early diagnosis of diabetic retinopathy significantly improves treatment outcomes and helps prevent permanent vision loss. Annual dilated eye exams are strongly recommended for:
- All individuals with type 1 diabetes (starting within 5 years of diagnosis)
- All individuals with type 2 diabetes (starting at diagnosis)
- Pregnant women with diabetes (ideally before conception and during each trimester)
Consistent control of diabetes, combined with regular eye screening, is the cornerstone of prevention.
Living with Diabetes: Protecting your vision
Maintaining eye health with diabetes requires a comprehensive approach:
- Keep blood sugar, blood pressure, and cholesterol within recommended levels
- Adhere to prescribed medications and treatment plans
- Maintain a healthy diet and stay physically active
- Avoid smoking and limit alcohol consumption
- Prioritise annual eye exams—even if your vision seems fine
Your eye health is closely tied to your overall diabetic management plan. By staying proactive, you can preserve your sight and prevent complications.
Conclusion
Diabetic Retinopathy is one of the leading causes of preventable vision loss in the working-age population. The good news is that with regular monitoring and timely intervention, vision loss can often be slowed, stopped, or even reversed.
At Moorfields Eye Hospital Dubai, our retina specialists provide expert diabetic eye care utilising the latest diagnostic technologies and advanced treatments to ensure each patient receives a tailored management plan.
Frequently Asked Questions (FAQs) about Diabetic Retinopathy
- Can diabetic retinopathy affect both eyes? Yes, diabetic retinopathy commonly affects both eyes. However, the degree of involvement may differ from one eye to the other. It’s not unusual for one eye to show more advanced damage while the other appears to be in an earlier stage. This asymmetry makes it essential for each eye to be evaluated separately during an examination. Since diabetic retinopathy can begin silently, even without noticeable symptoms, routine screenings by an ophthalmologist are critical for both eyes, regardless of how well a person may feel they are seeing.
- How long does it take for diabetic retinopathy to develop? The timeline varies from person to person. In individuals with type 2 diabetes, which often goes undiagnosed for several years, diabetic retinopathy may already be present at the time of diagnosis. In contrast, those with type 1 diabetes typically begin to develop changes in the retina after about five years of living with the condition. However, the onset and severity depend on how well diabetes is controlled. Factors such as persistent high blood sugar, unmanaged blood pressure, and elevated cholesterol levels can accelerate the progression of retinopathy.
- Can diabetic retinopathy be reversed?
Unfortunately, the structural damage caused by advanced diabetic retinopathy such as scarring, retinal detachment, or blood vessel closure is often irreversible. However, if diagnosed in its early stages, diabetic retinopathy can be managed effectively. Treatments like laser therapy, intravitreal injections, and surgical procedures can help preserve the remaining vision and prevent the disease from progressing further. Early detection offers the best chance for stabilising the condition and maintaining quality of life. - Does vision always improve after treatment?
Not always. The goal of treatment is to halt or slow down disease progression. While some patients do experience an improvement in vision, especially if they begin treatment early, others may not experience changes. For instance, if the macula (the central part of the retina responsible for sharp vision) has been affected, recovery may be limited. Nevertheless, stabilising the condition and avoiding further deterioration is a major success, particularly when intervention happens before irreversible damage has occurred. - Can I prevent diabetic retinopathy?
While it is not always possible to completely prevent diabetic retinopathy, its development and progression can be significantly delayed through good diabetes management. Keeping blood glucose levels within the target range, controlling blood pressure and cholesterol, avoiding smoking, staying physically active, and attending regular medical and eye check-ups all contribute to lower risk. People who consistently monitor and manage their diabetes tend to have milder forms of retinopathy and better long-term vision outcomes - How often should I have my eyes checked if I have diabetes? For individuals with diabetes, an annual comprehensive dilated eye exam is recommended. These exams allow ophthalmologists to detect changes in the retina before symptoms arise. If retinopathy is already present or if other risk factors exist such as pregnancy or poor diabetes control more frequent visits may be advised. Regular eye screenings are essential because diabetic retinopathy can develop and progress silently. Proactive monitoring helps ensure that any early signs are addressed before they escalate into vision-threatening complications
This blog on Keratoconus has been contributed by Dr Osama Giledi, Consultant Ophthalmologist, Specialist in Cataract, Cornea and Refractive Vision Correction Surgery
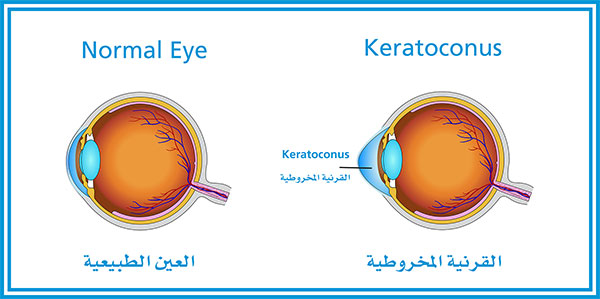
What is Keratoconus?
The word Keratoconus comes from two Greek words: kerato (cornea) and konos (cone). Keratoconus is a degenerative disorder of the eye in which the shape of the cornea, which is usually round, is distorted and develops a cone-shaped bulge, resulting in reduced vision. Keratoconus is a relatively common condition. It affects one person in two thousand, occurs around the world and is quite common in the Middle East.
Progression of Keratoconus depends on the patient’s age at the time of onset and the severity of eye rubbing. The earlier the onset, the faster Keratoconus may progress. The condition always affects both eyes and is asymmetric, so one eye may be more affected than the other.
Causes
Keratoconus has many causes, and it results in a cornea that is more elastic than normal and that starts to thin and bulge forward, causing reduced vision and increased astigmatism. It can be inherited, and a chromosomal link has been identified. Keratoconus can be associated with other allergic diseases such as hay fever, eczema and asthma but we are not born with it, and its onset usually happens around puberty. It is strongly associated with eye rubbing, making it progress rapidly. It is also seen in contact lens wearers.
For the best outcome, Keratconus should be detected and treated early. Early detection is possible by generating computerized corneal shape and thickness measurements through corneal topography using advanced technology such as a pentacam machine. If left untreated, Keratoconus could lead to significant visual impairment and blindness.
Treatment
Spectacles
These can provide good vision in the early stages of the condition and usually help to correct myopic astigmatism.
Hard or Scleral Contact Lenses
When spectacles don’t work, rigid contact lenses and Scleral lenses usually provide very good vision if the patient can tolerate them; they should be fitted by a contact lens specialist.
CXL – Corneal Collagen Cross linking with Riboflavin (Vitamin B2)
This technique increases the strength of the cornea and prevents the progress of Keratoconus.
Intracorneal Rings (Intacs & Ferrara)
These rings inserted into the cornea change the shape of the corneal cone, flattening it and making it a more regular and central shape. This will help improve the vision for the majority of patients.
We use it when patients cannot tolerate contact lenses and while the cornea is still clear and the condition is not very advanced. A Femto-second laser is used to create the tunnel and the entry point for the rings, making it a very safe and reliable procedure.
Toric Implantable Contact Lenses
For those with stable Keratoconus and good vision with glasses, Toric Implantable Contact Lenses are generally used (sometimes after stabilizing the Keratoconus with corneal cross linkage) to improve corneal shape with an intracorneal ring or with very limited therapeutic Excimer laser correction. The Toric ICL can eliminate the need for optical aids altogether and, in some patients, results in improved vision and balance between the two eyes.
Phototherapeutic Keratectomy (PTK)
Keratoconus patients are not candidates for Lasik or normal laser correction. However, some patients benefit from limited excimer laser correction to improve the surface irregularity of the cornea when
contact lenses cannot be tolerated. PTK is always combined with corneal cross-linkage, undertaken during the same procedure or afterwards.
Corneal Transplants
Corneal Transplants are used in the advanced stages of Keratoconus, when there is corneal scarring. The procedure is either a partial thickness (Deep Anterior Lamellar Keratoplasty = DALK) or full thickness graft (Penetrating Keratoplasty = PK). The need for corneal grafts is declining because of the increasing success in the early diagnosis of Keratoconus and the effectiveness of corneal cross linkage to stabilize the condition, so Keratoconus generally does not reach the advanced stage.