This blog on ‘Keratoconus and modern treatments’ has been contributed Dr. Osama Giledi, Consultant Ophthalmologist, Specialist in Cornea, Cataract and Refractive vision correction surgery.
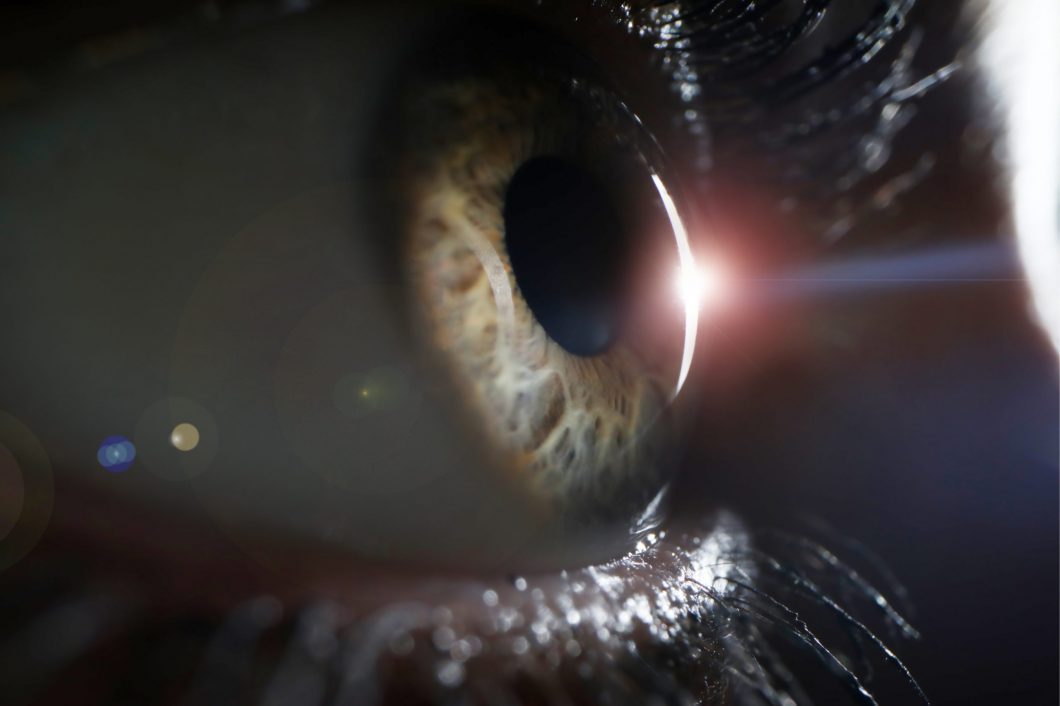
The cornea is the eye window which controls and focuses the entry of light into the eye, and in cases of keratoconus, there is a pathological decline in the thickness and rigidity of the cornea, which leads to irregular bulging of the cornea to a cone-like shape, which causes reduced vision from irregular astigmatism.
Corneal keratoconus usually affects both eyes and each eye may be affected differently, and usually occurs in people between the ages of 10 to 25 years. The condition may progress for 10 years or more and then slow down or stabilize. As the condition progresses, vision becomes distorted and blurred, with an increased sensitivity to light and glare.
Keratoconus presents itself in more certain ethnic groups, such as the Arab countries, southern Europe, and southern Asia. Environmental and genetic factors are potential causes, but the exact cause is uncertain.
Eye rubbing is a major risk factor. It is associated with some disease such as atopy and asthma. Also associated with some syndromes such as Down syndrome. If you have a family history of keratoconus, you have a greater chance of developing keratoconus. Pregnancy can make keratoconus progress more.
New corneal scans especially the 3 dimension scan such as pentacam help to diagnose Keratoconus at early stage.
Traditional treatment of keratconus was through glasses, hard contact lenses and corneal grafts. However, modern treatments for keratconus is used to stop the progress of Keratoconus, improve the shape of the cornea, and improve vision as well as avoiding the need for corneal graft.
Glasses or contact lenses can be used to correct nearsightedness and astigmatism in the early stages of keratoconus. As the Keratoconus progress, the patient needs a special solid contact lens.
Corneal collagen crosslinking
It is a procedure designed to halt the progression of keratoconus. The modern approach of accelerated pulsed crosslinking is used to ensure an easier procedure for the patient. We use ultraviolet A (UVA 360 nm), Riboflavin( vitamin B2) to stiffen and harden the cornea about four times and this stops the deterioration of keratoconus. The process is carried out under topical anesthesia and several drops of riboflavin are placed in the eye for about 15 minutes and activated by ultraviolet (UVA) rays for eight to thirty minutes. The corneal cross linakge is considered one of the safest and most successful operations used to stop keratoconus degradation and may lead to some improvement in some cases.
Intracorneal rings ( Ferrara, Kerarings or Intacus)
Intracorneal rings are plastic inserts that are implanted into the cornea to alter the shape of the cornea. It used to restore the regularity of the cornea again or at least reduce the irregularity; it will flatten the steepened section of a keratoconic cornea to achieve better unaided and better corrected vision. This often allows for a reduced prescription of spectacles and/or contact lenses and in some cases, satisfactory vision without glasses or contact lenses.
It is recommended to implant cornea rings in cases where the eyeglasses or contact lens are not able to clearly improve vision.
There ring can add strength to the cornea and it can be removed easily if it does not improve vision much.
The installation of rings using a femtosecond laser (intralase) added a new dimension to this type of operation. The process became safer and more effective and the femtosecond laser enabled the ophthalmologists to place these rings in the most accurate depth and diameter possible within the cornea with great accuracy and are way better than old Manual surgery. There are different sizes and thickness of rings depending on the shape of the keratoconus.
topography-guided laser surgery (TG-PRK).
Using topography guided eximer laser to improve the irregularity for the cornea surface in keratconus is a new method, where the patient who cannot tolerate contact lenses and has bad vision with glasses. The aim is to remove very little tissue so the patient can see clearly with glasses. There is a risk of weakening the cornea with this procedure, so we need to do a corneal cross linkage and minimize the amount of tissue removed by the eximer laser. Patient should be aware it is not to get rid of the glasses.
Implantable contact lens inside the eye.
It is used in patients with very high astigmatism and myopia who can see reasonably with glasses but the glass prescription are very high or has imbalance between the two eyes. These are placed inside the eye and have the ability to correct high degrees of short-sightedness and astigmatism. It is safe and effective procedure in selective patient, but the daily hard lens often provides for better vision than this lens as it corrects all the irregularity of the cornea.
Treatment with corneal cross linkage and intra corneal ring and topo guided laser all requires a minimum level of thickening of the cornea. Here the role of early diagnosis and treatment is highlighted, and that when the cornea becomes very thin these treatments become not possible, which makes corneal transplantation the only remaining treatment for such cases.
Corneal transplantation
It is recommended in advanced cases of keratoconus.
Out of all types of organ transplant surgeries (heart, lung, and kidney), corneal transplantation is the most widespread and successful of these.
We use modern ways to prepare the cut of both the donor and recipient cornea including using femtosecond laser.
There are various methods used for corneal transplant surgery. The old method includes removing the full thickness of diseased cornea and fixing the healthy cornea with stitches. As for following modern methods, the diseased frontal layers (DALK) is replaced and the patient retains the posterior portion of the cornea, thereby reducing the percentage of corneal transplants complications, especially the rate and severity of the corneal graft rejection.
Future treatment for keratoconus is prevention. Molecular genetics are currently being studied and we hope to identify people who are predisposing for the condition in an attempt to discover early and apply preventive treatment.
This blog has been authored by Dr. Miguel Morcillo, Consultant Ophthalmologist, Specialist in Cornea and Refractive Surgery.
What is Presbyopia?
When you have difficulty in focusing on near objects, usually as we head into our 40s & 50s, you probably are developing presbyopia. It is a condition that affects everyone as they get older.
Why presbyopia happens is not clear. When we are young we have a crystalline lens that is very flexible and the muscles within the eye can manipulate it so that it changes its shape, and therefore its power, so we can focus over a range of distances. This is a reflex and is done automatically without thought or effort. As we age, the lens becomes a stiffer, more rigid structure and it becomes harder for the muscles to get the lens to increase in thickness to become more powerful. As such, focusing up close becomes more problematic.
How does Presbyopia occur?
Presbyopia happens gradually. First, people start to put near objects a bit far, or increase the size of the font at the computer. It can work for few years but finally, the need for glasses to perform near activities appears. These glasses are magnifiers that can be used only for near in case the patient has good far vision, or may be added to the far glasses if the uncorrected far vision is not good. Presbyopia has been long time corrected with glasses but for those who don’t want to wear glasses, we have some surgical techniques available to correct this problem.
Treatment options for Presbyopia
Presbyopia surgery is not new. Monovision techniques are long time performed. They can be done either with laser or with intraocular lenses. The aim of monovision is to use the ability of the brain to process both eyes’ individual images to create the image we see. We call it binocularity. One eye is focused in far distance and the other eye is focused in near distance. Depending on the distance we focus, the brain chooses the best image as the principal image and uses the other eye as supporter of the main image. This combination is very useful in most of the daily activities and only in extreme far or small near activities, occasional use of glasses may be required. Monovision works quite well in myopic patients.
For those patients where monovision doesn’t match their expectations, we have multifocal intraocular lenses. These lenses are implanted after removing the natural lens. This is called refractive lens exchange. The multifocal intraocular lenses have different focuses to see in the most used near distances (mobile, books or computer screen) and also for far distances. They can be used in only one or both eyes, depending on the case. They can be implanted in cataract patients as well. Hypermetropic patients are most frequently implanted.
There are also some other techniques as corneal inlays, extended focus lenses or accommodative lenses. They may be used in some other cases but less frequently.
We select the technique depending on the age of the patient, the kind of glasses they are wearing, the current visual performance and the visual requirements. A complete eye check must be done to rule out any other pathology so the best results are obtained in healthy eyes. The results are excellent and most of the patients need no glasses at all. In few cases, it is possible some occasional use of glasses for specific activities. Even in these cases, we can provide high satisfaction levels to our patients and a change in their quality of life, where the continuous use of glasses before the surgery was very annoying for them.
This week’s blog on ‘Can astigmatism be cured?’ has been contributed Dr. Osama Giledi, Consultant Ophthalmologist, Specialist in Cataract, Cornea and Refractive Vision Correction Surgery.
What is astigmatism?
Astigmatism is a common kind of refractive error. It is not an eye disease, it means the surface of the cornea is not spherical, or not completely round “the eye is shaped like a Rugby ball, not a football ball.” With astigmatism, the eye does not focus light evenly onto the retina causing blurring of the image formed at the back of the eye.
Causes of astigmatism?
The specific cause is normally unknown although genetics can play a part. Sometimes astigmatism can develop after an eye injury, surgery or because of an eye disease Astigmatism is not caused by reading in bad light, using a PC or watching a lot of TV.
Astigmatism can affect both children and adults, it is usually non progressive and associated with myopia or hyperopia. If the astigmatism is getting worse, then it is very important to see a corneal specialist to a have corneal scan in order to rule out the weaker cornea (Keratoconus) as it is a progressive disease and there is treatment to stop it, especially if detected early, to save the vision.
What are symptoms of astigmatism?
Patients with astigmatism notice a blurred/distorted vision especially at night driving or have frequent headaches, increased eye fatigue, eye strain and squinting.
How is astigmatism diagnosed?
Astigmatism is usually found during eye glasses examination. Most of astigmatism are regular, however some astigmatism are irregular and caused by diseases affecting the cornea such as Keratoconus or corneal scar. Eye examination and a corneal scan is needed to rule out disease causing the astigmatism
Can you have astigmatism and not know it?
It is possible to have mild astigmatism and not know about it. This is especially true for children, who are not aware of their vision being other than normal. Some adults may also have mild astigmatism without any symptoms. Also many people wear glasses for myopia or hypermetropia and have mild astigmatism but were not informed about it.
Treatment: How is astigmatism corrected?
Astigmatism can be rectified with eyeglasses, contact lenses, or surgery.
Multiple ways of correcting astigmatism are:
- Eyeglasses are the simplest and safest way to correct astigmatism.
- Contact Lenses; need special Toric soft contact lens or hard contact lens.
- Refractive Surgery aims to correct astigmatism permanently in association usually with myopia or hypermetropia. There are various types of refractive surgeries to treat astigmatism using:
- Femto LASIK to change the shape of the cornea permanently
- Toric intraocular implant which we use in severe cases who is not suitable for laser vision correction or patient with weak cornea such as Keratoconus eye.
Astigmatism can also be corrected during cataract surgery by using toric intraocular implant so patient does not need to wear glasses after the procedure.
For astigmatism caused by corneal diseases, the treatment can be by different options depending on the disease and level of astigmatism. Options can be surgical cuts in the cornea (now by using femtosecond laser instead of knive), Eximer laser removal of irregular corneal surface and scar, insertion of specific intracorneal rings and lastly by replacing the diseased cornea with corneal graft
This week’s blog on ‘What your eyes tell you about your health’ has been contributed by Dr. Luisa Sastre, Specialist Ophthalmologist in Medical Retina.
“Do you have sleep problems?” the doctor asked while examining my eyes. “Yes, I do. How can you know that? “I replied in amazement.
Even though I slept well last night and my eyes were white and quiet, I still had that mild discomfort in my right eye that feels like a pricking sensation, right after I woke up.
The Doctor replied “I know because you have some very subtle punctate erosions on the surface of your inferior cornea. The pattern suggests that your eyelids could be open while you are sleeping and so the surface of your eye would be exposed to the environment and get dry”.
Then the doctor held my eyelashes and pulled a little bit. “You have loose elastic upper eyelids. They can easily open while you are asleep, causing the surface of your eye to get dry. That’s why you are getting this pricking sensation in your eyes, right when you wake up. As the day goes on, normal blinking will spread your natural tear over the surface of the eye, reducing the discomfort. Nonetheless, we would need to start a treatment plan to help treat this condition”.
The doctor knew very well the association between obstructive sleep apnea, floppy eyelid syndrome and the patient’s profile ; overweight, middle-aged male. The treatment recommended included not only eye lubricants, but a referral to the pulmonologist expert in sleep apnea and to the oculoplastic surgeon.
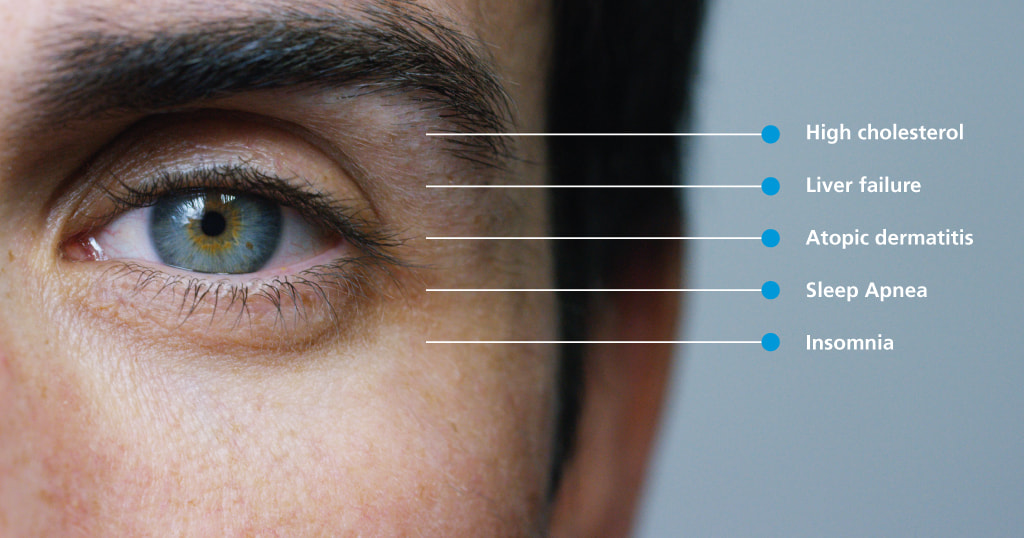
This is just an example of an association between eye conditions and other problems in any part of your body. Some of these classical associations are diabetes and hypertension. The eye doctor can tell how good or bad your sugar or blood pressure control has been, just by looking inside the eye, through that little window called the pupil. Indeed every diabetic person should have regular eye examinations, with dilation of the pupil, to assess the retina’s health.
In the same way itchy red eyes can come along with flare ups of certain skin conditions, like atopic dermatitis or rosacea.
People under a lot of stress and those with sleep disturbances like insomnia or type A behaviour (aggressive and competitive personalities) are more likely to develop a condition in the eye called central serous chorioretinopathy (CSC). CSC can significantly impair your vision. So your eye doctor once again, will not only give you appropriate advice for your eyes, but also refer you to a sleep expert or to a psychologist, in order to have a comprehensive approach to your problem.
Examples of common associations:
- If you suffer a sudden drop in your vision and you are diagnosed with a vascular occlusion in your retina, you could be found to have high cholesterol and other cardiovascular conditions. So a prompt correction of your cholesterol levels can save you from future threats such as a heart attack and brain stroke.
- Not being able to see in a certain part of your visual field could mean a tumor might be compressing certain structures in your brain.
- If the whites of your eyes get yellow, you could have liver problems.
- If your eyes are red, painful and your vision is impaired and you are diagnosed with a condition called uveitis, you could also be found to have rheumatic diseases.
The list can go on, hence the Conclusion is; visit your eye doctor regularly as he/she is much more, than just an eye doctor!!
This blog on ‘Amblyopia (lazy eye)’ has been contributed by Dr. Suhair Twaij, consultant ophthalmologist in Adult & Paediatric Strabismus Surgery, General Paediatric Ophthalmology, Adult Cataract Surgery & General Ophthalmology
What is Amblyopia?
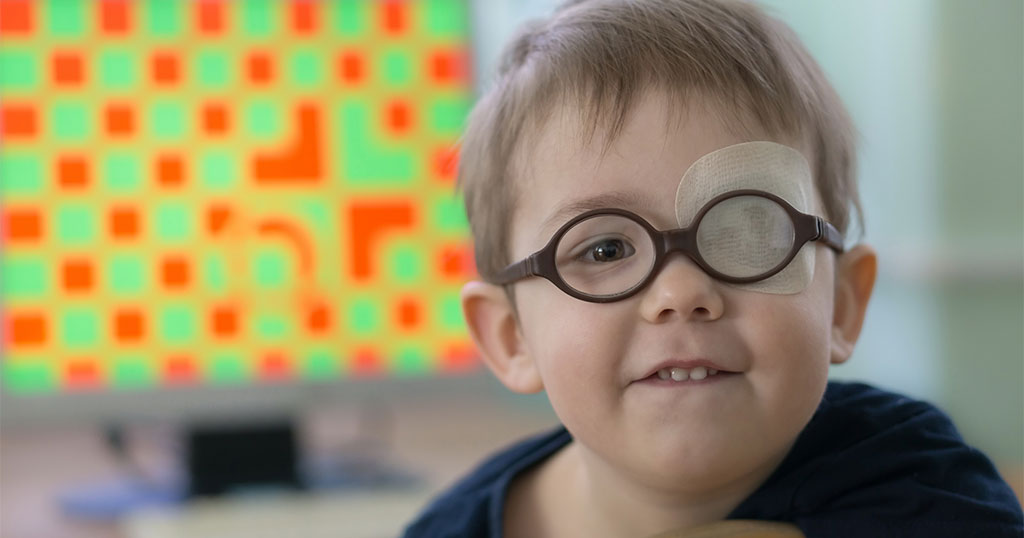
The most common cause of a visual deficiency in children is amblyopia or lazy eye. It occurs when the eye fails to work with the brain properly.
Although the eye may appear normal, the brain prefers the other eye. This can happen in the critical period of eye development, which is from birth until about age 7, when children’s eyes and the brain form vital connections. These connections can be blocked or prevented by anything that obstructs or blurs vision in one or both eyes, leading to lazy eye. Sometimes both eyes may be affected.
Causes
A number of things can interfere with normal brain–eye connections and lead to amblyopia;
- Strabismus (squint): a disorder in which the two eyes don’t line up in the same direction.
- Refractive errors: when one eye cannot focus as well as the other. This includes nearsightedness, farsightedness and astigmatism.
- Cataract: a clouding in the lens of the eye.
- Droopy lid.
- Genetics play a role, too. Amblyopia tends to run in families. It’s also more common in children born prematurely or those with developmental delays.
Unfortunately, most children with amblyopia won’t complain of vision problems. Often, a parent or teacher might realize that a child is struggling with a vision problem, maybe noticing crossed eyes, frequent squinting, or tilting the head to see better. Some kids have poor depth perception (trouble seeing in three dimensions), difficulty with sports and clumsiness.
Diagnosis
Regular vision examinations by medical specialists are crucial for identifying any issues in children. To detect issues before a kid reaches visual maturity, these assessments should begin in the toddler and preschool years.
Treatment
As soon as possible, treatment should begin. The purpose of the treatment is to have the child use the eye with poorer vision. This is accomplished with eyewear, surgery, eye drops, eye patches, eye patches, or a combination of these.
This week’s blog on ‘Bell’s palsy’ has been contributed by Dr Osama Giledi, Consultant Ophthalmologist, Specialist in Cataract, Cornea and Refractive Vision Correction Surgery
What is Bell’s palsy?
Bell’s paralysis known as Bell’s palsy is a temporary weakness or lack of movement affecting one side of the face. It is the most well-known type of facial paralysis
Symptoms
Bell’s palsy affects the function of facial muscles, as well as tears, saliva, taste and the middle ear. It appears as droopiness on one side of the face from weakness or total paralysis of the facial muscles and it develops within two days.
The symptoms of Bell’s palsy include:
- Sudden limitation or loss of motion on one side of the face
- Drooping eyelid or corner of the mouth
- Difficulty smiling or shutting the eyelid
- Ear pain
- Drooling
- Dryness in the eye and mouth
- Ringing in the ear or sensitivity to sound
- Impaired speech or taste
- Reduced tear production.
If you have any symptoms of Bell’s palsy, it is advised to consult your physician early.
However, if facial weakness is a symptom in a person who cannot lift up both arms and keep them there or have difficulty speaking (speech may be slurred or garbled) you need to go to emergency department as these can be signs of a more serious condition, like a stroke. In contrast to Bell’s palsy, the symptoms of a stroke are sudden.
Treatment
Bell’s palsy is usually treated by a General practitioner. Symptoms generally begin to diminish within two weeks of starting treatment, with complete recovery within half a year
Treatments for Bell’s palsy include:
- A Short 10-day course of Oral steroid (medication should be within 3 days of the symptoms starting to speed the recovery of bell’s palsy)
- Eye drops and eye ointment to protect the eye and to stop the affected eye from drying out
- Surgical tape to keep the eye shut at bedtime
Bell’s palsy is rare in kids, and most kids who are affected make a full recovery without treatment.
How long the Bell’s palsy lasts
Most patients recover fully within 6 months, but sometime it can take longer. In a small number of cases, the facial weakness can be permanent which can be treated by surgery.
Causes and Risk Factors
Bell’s palsy is caused by inflammation or compression of the facial nerve (Seventh cranial nerve), which controls face muscles. Infection by a virus is believed to cause inflammation and swelling of the nerve. Various viruses from the herpesvirus family are related with Bell’s palsy. Other Non-Viral causes such as: Headaches, chronic ear infection, tumors, diabetes and injury to the face.
You can’t prevent Bell’s palsy
Because it’s probably caused by an infection of several types of viruses, Bell’s palsy cannot be prevented.
You’ll normally just get Bell’s paralysis once, yet it can once in a while return. This is more probable in the event that you have a family history of the condition.
Retinoblastoma is an eye cancer that occurs most commonly in childhood under the age of 5. . Two thirds of children are diagnosed before the age of two and almost 95% by the age of 5.
It is estimated that 5000-8000 children develop retinoblastoma worldwide every year. The incidence rate of retinoblastoma in United States and Europe is approximately 1:15000 live births. However, the rate appears to be higher in Africa and India.
Its present in two forms, bilateral (hereditary) form (25% of all cases) and unilateral (75% of all cases, 90% of which are non-hereditary).
The most common presentation is leucocoria which is an abnormal white reflection in the eye (60%) and 20% as squint, the misaligned position of the eye).
The best approach to manage this condition is based on early detection and early diagnosis.
It involves Paediatric Ophthalmologist, Ophthalmic Oncologist and Paediatric Oncologist. The aim of the treatment is primarily to preserve the life of the child. Secondly, to preserve vision and finally, to preserve the eye. It is highly curable if identified in early stages; more than 90% of children survive in high income countries and up to 40% in less privileged countries. Treatment includes radiotherapy, chemotherapy and sometimes enucleation of the eye with tumor. Children with bilateral disease and gene mutation are at higher risk for secondary cancers. This increases with radiation therapy.
It is very important to for parents, Pediatricians, Ophthalmologists and other healthcare professional involved in childcare to detect abnormal white reflection (absence of red reflex) during routine checkups of the children.
Leucocoria can be seen in the eye with the tumor due to the reflection of the white flash light from abnormal white retina in the back of the eye.
In the modern phone cameras, a red eye reduction feature is included so that the red reflex is prevented in the photos. There are few iPhone applications (apps) which are designed to detect the white reflex. However, there are certain limitations with these apps.
A thorough eye examination by a Paediatric Ophthalmologist is essential to detect the tumor in its early stages when concerns arise by parents with these apps or iPhone photos.
Why is it important for children to wear sunglasses?
As children are in a dynamic active state of growth, it is estimated that 50% of total sun exposure occurs in the first 18 years of age, since children are more active outdoor during this age. Another important factor is the deletion of the ozone layer, a protective filter layer of atmosphere, leading to increased exposure to UV radiation which can negatively affect children’s skin and eyes.
UVA rays may cause harm to the central vision, causing damage to the macula, a central part of the retina at the back of the child’s eye. UVB may cause harm to the front part of the eye (cornea and lens), which absorb UVB rays. The other well-known side effects of UV radiation include: cataract (clouding of lens), macular degeneration, pterygium (benign growth on the white of the eye) and corneal sunburn which is painful and might cause temporary vision loss. Additionally, blue rays may cause digital eye strain due to the high energy light that is emitted by computer and mobile phone screens. Another important fact is that children’s eyes are more susceptible to the harm caused by excessive exposure to UV rays than adults because the young clear lens inside the eye is less capable of filtration of these harmful rays.
To put things in perspective, normal light is between 400 nm (on the blue end of the spectrum) to 760 nm (on the red side). However, the sun emits other electromagnetic waves in addition to light. The sun emits two types of ultraviolet rays (UV) radiation, UVA (ranges between 320-400 nm) and UVB (ranges between 290-320 nm). UVA accounts for about 95% of the UV radiation that reaches the skin and eyes. UVA rays are considered to be more harmful than UVB since they penetrate farther into skin and eyes than UVB. Also UVA rays penetrate glass while UVB rays do not. Both UV rays are reflected from sand, water and snow (80% of UVB rays reflect from snow).
In conclusion, it would be very wise for parents to ensure that their children wear protective tinted sunglasses outdoors, especially in snowfields, sandy beaches and near pools and sea. The color of sunglasses is not correlated with the level of UV protection, thus special tinted glasses with certification that will block up to 100% of the sun’s UV radiations is needed. However, before buying these sunglasses, it is advisable to arrange an eye examination with Paediatric Eye Doctor for a thorough eye examination and to provide a prescription for the glasses, if needed.
This blog on Minimally Invasive Glaucoma Surgery (MIGS) was authored by Dr. Salman Waqar, Consultant Ophthalmologist in Cataract and Glaucoma Surgery.
What is MIGS?
Minimally Invasive Glaucoma Surgery, or MIGS, has shown formidable results in mild or moderate glaucoma. MIGS is designed to improve the safety of surgical intervention for glaucoma cure.
While coined minimally invasive, micro is a more appropriate term, truly differentiates these microscopic ophthalmic procedures from other minimally invasive surgical procedures (i.e., general surgery). MIGS can be considered as an alternative to medical therapy in an effort to address adherence challenges, adverse events, and quality-of-life (QOL) issues with topical medications.
The iStent
The iStent is the smallest implantable device approved by the FDA to be used on the human body. The iStent can reduce the need for daily use of glaucoma eye drops. A small (1mm) titanium drainage stent is inserted into the eye’s natural drainage channel to lower intraocular pressure.
The iStent is not visible in the eye, and shows no physical evidence of its presence. Nor does it appear in the vision of the person with the stent.
XEN Glaucoma Implant
The implant is a soft, collagen derived, gelatin that is known to be non-inflammatory. The Xen Gel Stent aims to reduce intraocular pressure by inserting a small drainage tube into the eye. The stent allows fluid to drain from the anterior chamber into a reservoir (bleb) under the conjunctiva. The goal of implantation is to create an aqueous humor outflow path from the anterior chamber to the subconjunctival space.
Similar to the iStent, the implant also has no physical appearance. However, occasionally a shallow bleb can be seen in extremes of gaze, where the eye is looking very far down and outwards.
The Surgery
Successful MIGS surgery takes much less time than many other types of Glaucoma surgery, typically lasting 30 minutes at the most. At Moorfields Eye Hospital Dubai/Abu Dhabi, MIGS implantation is usually performed under local anaesthesia, although general anaesthesia is also possible under certain circumstances.
Typically a drug called Mitomycin C (anti-scarring medication) is also used at the time of surgery if indicated to suppress healing.
It is extremely rare for complications to occur at the time of the surgery. When the complications do occur, they occur usually within 2 weeks of the surgery.
Postoperative Period
The blurring is usually worst for the first 1 to 2 weeks after surgery, and improving slowly afterwards. It takes about 1 month for the eye to feel completely normal though vision would stabilise much earlier.
Eye drops and tablets to lower the eye pressure are not normally required for the operated eye during the first night after surgery. The following day, the postoperative eye drops are usually started after removal of the eye patch and cleaning of the eye. The postoperative eye drops will usually consist of an antibiotic and anti-inflammatory steroid eye drops to use for the first month after surgery.
The patient will require two follow up visits two weeks apart, after the operation in order for a follow up.
Following surgery you are able to read and watch television as normal as these activities will not harm your eye. It is however important to avoid strenuous activity during the first few weeks after surgery.
Here is a table with the dos and don’ts:
| Activity | Advice |
| Hair Washing | No need to avoid but back wash advised to avoid getting shampoo into your eye. It may be easier to have someone else wash your hair for you. |
| Showering/Bathing/Wadhu | No need to avoid but don’t allow soapy/dirty water to go into your eye |
| Sleeping | Try to sleep on your un-operated side. Tape the plastic eye shield provided over your eye every night for two weeks to avoid accidentally rubbing your eye whilst asleep. |
| Walking | No restrictions |
| Wearing glasses/sunglasses | Do not change the prescription of your glasses until the doctor advises. You may wear sunglasses for comfort and UV protection. |
| Driving | Your doctor shall advise you. If advised against driving and you continue to do so, this shall be at your own risk. |
| Flying | No restrictions |
| Going away on holiday | Discuss with your doctor/nurse as it is very important to attend your follow up appointments. |
| Wearing eye makeup | Avoid for one month then use new makeup. Never share eye make-up with anyone else. |
| Household chores e.g. cleaning, ironing, hovering | Avoid for 1 – 2 weeks |
| Sexual Activity | Avoid for 1 – 2 weeks |
| Gym workout | Avoid for 1 months |
| Playing any sport | Avoid for 1 months |
| Running/jogging | Avoid for 1 months |
| Swimming | Avoid for 1 months, after which you must use goggles |
| Prayers (Salah) | You may continue prayers but do the rockoo/sajdah in a chair, your head must not go below your heart level. |
With showing 80-90% success rates in most studies, MIGS is slowly becoming a well requested form of glaucoma correction, especially since it only takes around 1 month for the eye to feel completely normal in most cases.
This week’s blog on Are all LASIK procedures the same? Which one is the best? has been contributed by Dr Osama Giledi, Consultant Ophthalmologist, Specialist in Cataract, Cornea and Refractive Vision Correction Surgery
If you have been thinking about laser vision correction surgery and reading up on it, you may have come across many different procedure names. Some may say that it is very confusing to understand and compare them to one another, especially as there are different packages and prices offered for such procedures.
The two main types of refractive laser procedures are the LASIK procedure and the surface laser procedure.
The LASIK procedure is one in which the thin layer of the cornea (located in the front part of the eye) is created, called a flap. The flap is then lifted to allow for the application of excimer laser energy beneath it. The laser then reshapes the cornea for vision correction outcomes. After the laser treatment is completed, the protective flap is replaced back to its original place in order for it to heal.
With traditional LASIK, a mechanical instrument called a Microkeratome uses a moving blade to create a thin corneal flap. Traditional LASIK may cause complications such as torn flaps and free flaps which in some cases can unfortunately cause permanent reduced vision. It is also known as Ultra LASIK, SupraLASIK or Thin LASIK.
An alternate new method of creating a LASIK flap is through the use of a femtosecond laser, also known as “IntraLase,” “blade-free” or “all-laser LASIK.” This technology represents an innovative and highly sophisticated laser technique used to prepare the cornea for laser vision correction surgery. This allows extra safety for the laser procedure. Using laser technology to create the corneal flap, which is most important step in LASIK procedure, has made the procedure much precise, effective, eliminates serious flap creation risks and is arguably the safest LASIK technique to undergo. Femtosecond lasik allows the surgeon to choose a excellent centration of the flap, create precise diameter and thickness and edge design of the flap, so it improves both the quality and the accuracy of the procedure.
A result, this reduces the risk of surgical flap formation complication to almost risk free, also reducing the risk of post-surgery flap wrinkles and weaker cornea, and also reduces the risk of dry eye after the procedure.
LASIK was originally approved by the FDA in 1995. The first FDA-approved bladeless flap-making system in the United States was in 2007, so it is not a new procedure, but as technology has advanced over the years, it is now extremely precise, safer and easy to perform with predictable outcomes.
In conclusion, not all LASIK procedures are equal; if you are considering LASIK, ask your surgeon whether they will perform the blade or Femto laser LASIK flap. If price is a major concern for you, the blade procedure may provide an option, however you should also consider the safety and raised potential complication rates and risks associated with this. Using the femto laser flap technique, your risk of complications and outcomes are much better guaranteed to be in your favor and also remember that some facilities offer different packages and financing options.
The choice is yours, just make sure to ask your surgeon, and the facility you are seeking treatment from, enough questions, especially how the Lasik flap is created in order for you to make an informed decision.
This week’s blog on Smoking and the eyes has been contributed by Dr Ammar Safar, Medical Director, Consultant Ophthalmologist and Vitreoretinal Surgeon.
Most people are very aware that smoking in all shapes can cause cancer, lung and heart disease, as well as many other health problems but people are always surprised when I tell them that smoking can seriously affect the health of their eyes too.
Here are some of the more important eye conditions affected by smoking:
- Dry eyes: This is a very common condition especially in the gulf area and it can be severely aggravated by smoking. Patients will feel burning sensation, scratchy eyes, redness, sandy sensation and severe irritation.
- Macular degeneration: this is a vision threatening condition that affects people over age 55 and can cause severe distortion or loss of central vision. Smokers are 4 times more likely to get this condition than non-smokers and people who live with smokers are 2 times as likely to get it too. Recent medical improvements have introduced a treatment for the severe form of AMD in the form of injections in the eye to restore vision loss. Research has proven that smokers are much less likely to respond to these injections than non-smokers.
- Cataract: This is clouding of the natural lens of the eye that obstructs vision. People who smoke are 2 times more likely to get cataract than those who do not.
- Diabetic retinopathy: People who are diabetic and smoke have much more risk of developing problems in the retina called diabetic retinopathy. This can be a serious condition and lead to blindness.
- Smoking while pregnant: If you smoke while being pregnant you could increase your child’s risk of bacterial meningitis by 5 folds. This condition causes swelling around the tissue of the brain and can seriously affect the eyes and the optic nerve. In addition to that, smoking during pregnancy increases the risk of early delivery. This can have direct effect on the eyes and especially on the retina. This condition is called Retinopathy of Prematurity (ROP) which is a serious condition, if left untreated can lead to permanent vision loss.
Patients are advised to engage in programs that lead to quitting this dangerous habit. Studies have shown that patients who quit smoking reduce their risks to pre smoking levels after 5 years of quitting.
This week’s blog on Blue light has a dark side has been contributed by Dr Osama Giledi, Consultant Ophthalmologist, Specialist in Cataract, Cornea and Refractive Vision Correction Surgery
What is blue light? The effect blue light has on your sleep and your health
Visible light is a lot more complicated than people may think.
Phones, tablets, televisions, electronic devices, LED lighting, streetlights, and even energy efficient light bulbs in your home; almost everything we interact with during the day emits blue light – including the sun shining above us.
We’re exposed to a broad spectrum of different kinds of visible (and sometimes invisible) light that can have a range of effects on your health. From retinal damage to a potential loss of vision, blue light is a risk to our health and should be considered.
Blue light is the portion of the visible light spectrum with the shortest wavelengths and highest energy ranging from 380 to 500nm. The sky looks blue because of blue light wavelengths from the sun.
The sun’s blue light regulates our body’s natural wakefulness and sleep cycle, called the circadian rhythm. Blue light affects melatonin production, the hormone that controls the circadian rhythm.
When the sun comes up in the morning, melatonin production comes to a natural halt and when it sets production starts back up again, telling the body to prepare for sleep and restoration, so we can refuel for the day ahead.
When we look at our electronic devices late at night, our melatonin production is reduced as a result. This is because blue light signal your pineal gland to stop producing melatonin. To your brain, blue light registers similarly to natural daylight, “tricking” your body to become more awake and alert which may cause sleepless nights and daytime fatigue.
Our circadian rhythms are naturally designed to synchronize with the rising and setting of the sun meaning that when the sun is out, our mind and bodies are alert and awake.
But circadian rhythm controls more than your sleep. This body rhythm regulates dozens of bodily functions like hormones, cellular health, blood sugar levels and metabolism and possibly even more functions we aren’t aware of yet.
Melatonin suppression has been linked with sleep disorders, increased diabetes, obesity, heart disease and even some forms of cancer.
When we aren’t in tune with our biological clock, our system begins to wear down, leaving us vulnerable to disease.
As technology improves, the amount of digital consumption through personal devices increases. The ease at which users are able to watch a movie on their phone or tablet, holding the screens in such close proximity to their eyes could mean potential long term damage to their eyes.
The eye is not very good at blocking blue light, especially in children. With age our lenses absorb some of the blue light and reduce the amount of blue light that reaches the retina.
Some blue light exposure can also be good for your health. Studies have shown that blue light exposure can boost your bodies alertness, help memory and even lift your mood. Light therapy has even been used to help with the treatment of depression.
Blue light can also contribute to digital eye strain, because short-wavelength, high energy blue light scatters more easily than other visible light, which means it isn’t as focused.
When you look at your television or laptop screen, your eyes are looking at unfocused visual “noise”.
These unfocused wavelengths are stressful on the eyes because they must constantly focus and re-focus on these flickering waves in our visual field. This creates glare or fuzziness in your vision, which is a common cause of headaches, fatigue, and eyestrain.
How can we combat the negative effects of prolonged exposure to screens?
Blue light blocking glasses and lenses have been developed to combat the effects of prolonged exposure to blue light. However, studies have shown that these lenses may increase contrast significantly. For a more comfortable experience when looking at a digital device for extended periods of time, yellow tinted lenses can be used to reduce strain on your eyes.
Researchers suggest that prolonged exposure to blue light could cause progressive destruction of retinal cells in the eyes therefore contributing to age-related macular degeneration, which is one of the leading causes of blindness.
Alternatively, nearly all visible blue light reaches the retina through the cornea and lens. For people who have cataracts and are about to have surgery, you can have an intraocular lens (IOL) surgically implanted with in-built blue light protection.
What about prolonged phone use?
If you are using your phone a lot, a convenient way to reduce your blue light exposure is to use a blue light filter. The blue light filter function is featured in some devices’ display settings and available to download from the relevant app stores. This filter limits the amount of blue light reaching your eyes without affecting the quality of the resolution and display. These are available for most modern digital devices including smartphones, tablets and computers and help to reduce the amount of blue light produced reaching your eyes.
Even better, stop using digital devices for a while before going to sleep.
Look for bulbs with opaque coatings to reduce bright light emissions. Or better yet, find a dimmable or colour-changing bulb that allows for softer light in the evening.
You can also use a dimmer on your tech screens. The mobile operating system activates blue light filtering at night. (Images: Apple Inc.)
Also, you can use some applications such as fl.ux for computers and laptops to reduce the light emitted from your devices and adjust it for the time of the day.
Computer users and those who work night shift can protect themselves by wearing blue light blocking glasses.
A Harvard study found evidence that blue-light blocking goggles are effective against the melatonin suppression response of blue light. Night shift workers are especially encouraged to invest in blue-light blocking goggles
https://www.health.harvard.edu/staying-healthy/blue-light-has-a-dark-side