This blog has been contributed by Dr. Ammar Safar, Consultant Ophthalmologist and Vitreoretinal Surgeon and Chief Medical Officer.
Artificial intelligence (AI) has revolutionised various industries, and it’s making its way into ophthalmology. AI technologies are being viewed as valuable tools for diagnosing, managing, and treating eye diseases.
AI algorithms can analyse large amounts of data in a short time, making it easier to identify and treat eye conditions. One of the most significant applications of AI in ophthalmology is in detecting and diagnosing retinal diseases, including diabetic retinopathy, age-related macular degeneration, and glaucoma.
Diabetic retinopathy is a leading cause of blindness in adults. It is unfortunately very prevalent in our part of the world with a large number of patients affected. However, with the help of AI, ophthalmologists can now detect the disease early and provide timely treatment. AI-powered retinal imaging systems can analyse a large number of retinal images for early signs of the disease with an outstanding level of accuracy, providing ophthalmologists with a more accurate diagnosis and making it next to impossible to delay or miss a diagnosis.
Age-related macular degeneration is another eye condition that can lead to vision loss. AI algorithms can analyse the retina’s images to detect signs of the disease and track its progression, enabling ophthalmologists to provide appropriate treatment.
Glaucoma is a condition that damages the optic nerve, leading to vision loss. AI technologies can detect the disease in its early stages, allowing for early intervention to prevent further vision loss. AI algorithms can analyse visual field tests, imaging tests, and other data and compare them to previous tests detecting even the very minute variations providing a very powerful tool to determine the likelihood of developing glaucoma and its progression.
AI can also assist ophthalmologists in the management of cataracts, which is a common cause of vision loss in older adults. AI algorithms can analyse patient data, including medical history, to determine the appropriate surgical approach and intraocular lens power.
AI technology has the potential to revolutionise ophthalmology, enabling ophthalmologists to provide more accurate diagnoses and personalised treatment plans. While AI cannot replace human expertise, it can significantly enhance it, providing ophthalmologists with a powerful tool to improve patient care.
In conclusion, AI can transform ophthalmology by improving the diagnosis, management, and treatment of eye diseases. As technology advances, AI will undoubtedly become an increasingly essential tool for ophthalmologists.
This blog has been contributed by Dr. Salma Yassine, Consultant Ophthalmologist in Paediatric & Neuro-ophthalmology
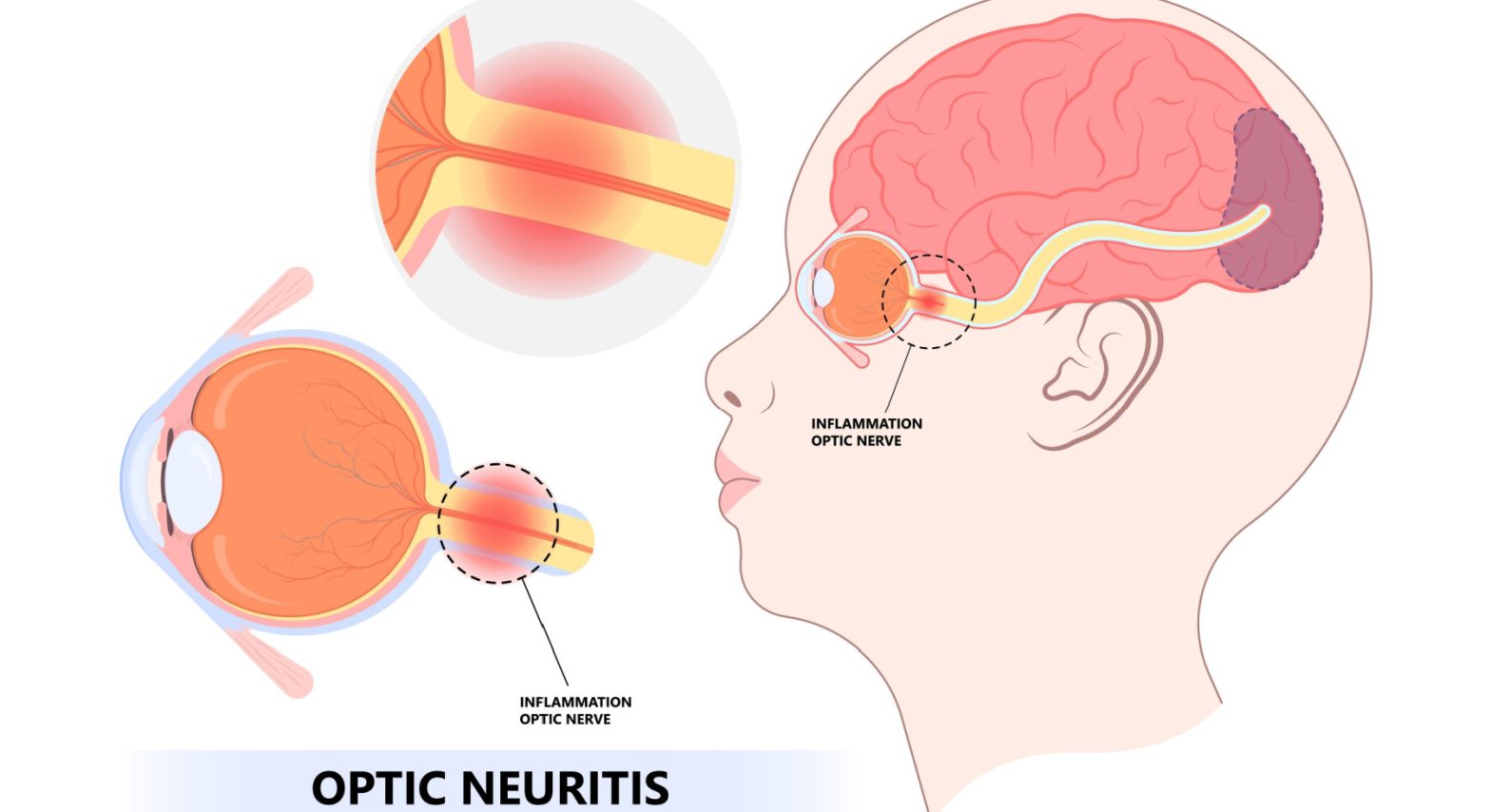
What is optic neuritis?
Optic neuritis occurs when our immune system mistakenly targets the substance covering your optic nerve, resulting in inflammation and damage to the myelin. This disrupts electrical impulses that travel from the eye to the brain, causing blurred or dark vision.
How does optic neuritis affect me?
Optic neuritis usually affects one eye. Symptoms might include:
- Pain: Eye pain that’s usually worsened by eye movement. Sometimes it presents as a dull ache behind the eye.
- Vision loss in one eye: Noticeable vision loss usually develops over hours or days and improves over several weeks to months. However, vision loss can be permanent in some people.
- Visual field loss: Central or peripheral vision loss
- Loss of colour: Colours appear less vivid
What causes optic neuritis?
The following autoimmune conditions often are associated with optic neuritis:
- Multiple sclerosis: It is a disease in which the autoimmune system attacks the myelin sheath covering nerve fibres in your brain. The risk of developing multiple sclerosis after optic neuritis increases further if an MRI scan shows demyelinating brain lesions
- Neuromyelitis Optica: In this condition, the inflammation affects the optic nerve and spinal cord. As a result, it often results in diminished visual recovery after an attack compared with MS.
- Myelin oligodendrocyte glycoprotein (MOG) antibody disorder: Like neuromyelitis optica, recurrent attacks of inflammation can occur in the optic nerve, spinal cord or brain. However, recovery from MOG attacks is usually better than recovery from neuromyelitis optica.
When symptoms of optic neuritis are more complex, other associated causes need to be considered, including infections, rheumatological diseases, and drugs or toxins (ethambutol or methanol)
Why do I need to see a neuro-ophthalmologist?
- Neuro-ophthalmologist is experienced in sorting out the differences between optic neuritis and other optic nerve diseases.
- During your office visit, the doctor will check your visual fields and scan your optic nerves
- Your doctor will order an MRI of the brain with special views of the orbits with contrast to confirm optic neuritis
- Your doctor may order other tests, such as blood tests or a chest X-ray
What are the possible complications?
- Optic nerve damage: Most have permanent optic nerve damage after an episode of optic neuritis, but the damage might not cause permanent symptoms.
- Decreased visual acuity: Most people regain normal or near-normal vision within months, but a partial loss of colour discrimination might persist.
Side effects of treatment: Steroid medications used to treat optic neuritis suppress the immune system, which causes your body to become more susceptible to infections. It can also cause mood changes and weight gain.
This blog has been contributed by Dr. Salman Waqar, Consultant Ophthalmologist in Cataract and Glaucoma Surgery at Moorfields Eye Hospital Dubai.
Cataracts are one of the most common causes of gradual vision change as we age. In Dubai and across the UAE, many people first notice subtle symptoms that are easy to dismiss, such as a slight blur, increased glare when driving at night, or colours that no longer appear as vivid as they once did. Over time, cataracts can begin to interfere with daily activities such as reading, driving, recognising faces, or using digital devices.
Understanding what cataracts are, how they develop, and how they are treated can help you recognise symptoms early and make informed decisions about your eye health and treatment options.
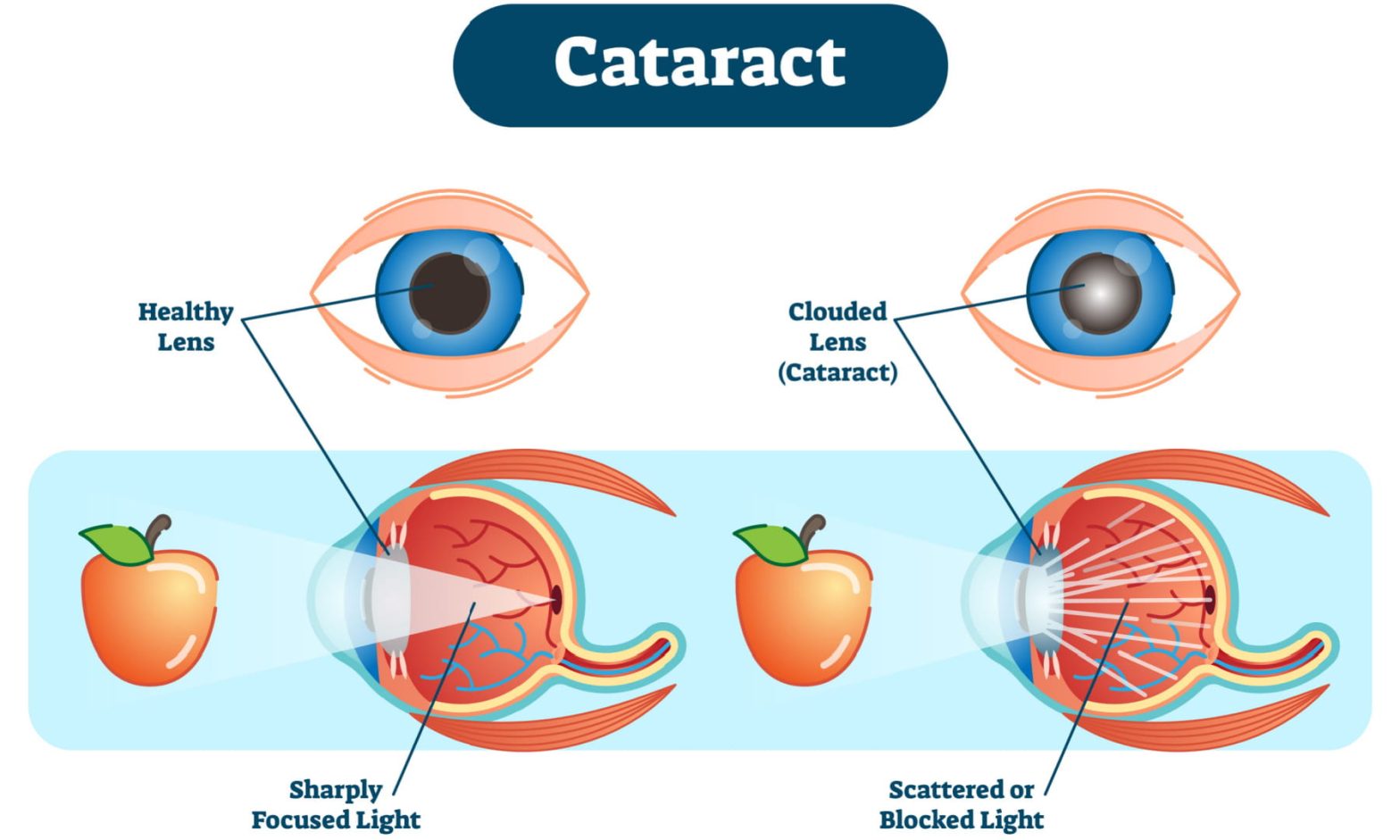
What are cataracts?
Inside each eye sits a clear, flexible structure called the lens. The lens focuses light onto the retina, allowing the brain to form clear images. In a healthy eye, the lens is transparent, enabling light to pass through without distortion.
A cataract occurs when this lens becomes cloudy or opaque, preventing light from passing through clearly. As a result, vision becomes blurred, hazy, or dim, much like looking through a fogged or scratched window.
Cataracts typically develop slowly and painlessly, which is why many people do not notice the change immediately.
Why do cataracts develop?
The most common cause of cataracts is ageing. Over time, the proteins within the lens begin to break down and clump together, reducing the lens’s clarity. This process is a natural part of ageing and affects most people to some degree.
Globally, cataracts remain a significant cause of vision loss. According to the World Health Organization (WHO) and data referenced by the National Institutes of Health (NIH), untreated cataracts are the leading cause of blindness worldwide, accounting for approximately 50–51% of global blindness, particularly in older populations.
Cataracts are also a major eye health concern in the UAE. As mentioned by the National Institutes of Health (NIH), a population-based visual impairment survey conducted in Dubai found that cataracts were responsible for approximately 17.2% of visual impairment cases among adults, making them one of the leading causes of reduced vision in the local population.
In addition to age, other factors can contribute to cataract development, including:
- Diabetes, which is prevalent in the UAE
- Prolonged exposure to ultraviolet (UV) light
- Smoking
- Certain medications, such as long-term steroid use
- Eye injuries or trauma
- Previous eye surgery
What are the types of cataracts?
While age-related cataracts are the most common, cataracts can develop for different reasons and at different stages of life:
- Age-related cataracts: These develop gradually as part of the natural ageing process and are the most frequently diagnosed type in Dubai and the wider UAE.
- Congenital cataracts: Present at birth or developing in early childhood, often due to genetic factors or infections during pregnancy.
- Traumatic cataracts: Caused by eye injury, which may lead to cataract formation immediately or years later.
- Secondary cataracts: Develop as a result of other eye conditions, systemic diseases, or medications.
Regardless of the type, the impact on vision is similar, and management depends on how much the cataract interferes with daily life.
What are the symptoms of cataracts?
Cataracts do not develop overnight. Symptoms often progress gradually and may include:
- Blurred or cloudy vision
- Increased sensitivity to glare, especially from headlights or bright sunlight
- Halos around lights
- Difficulty seeing at night
- Colours appearing faded or yellowed
- Double vision in one eye
- Frequent changes in glasses or contact lens prescriptions
As cataracts progress, these symptoms become more noticeable and can significantly affect quality of life, particularly for those who drive frequently or use digital screens for work in a fast-paced city like Dubai.
Does cataract threaten vision?
Cataracts do not damage the eye itself, and vision loss caused by cataracts is reversible. However, if left untreated, cataracts can eventually lead to significant visual impairment, affecting independence and safety.
How are cataracts diagnosed?
Cataracts are diagnosed through a comprehensive eye examination. This includes:
- Assessment of visual acuity
- Examination of the lens using a slit lamp microscope
- Evaluation of the retina and optic nerve
- Measurement of eye pressure
- Detailed discussion of symptoms and daily visual needs
Not all vision changes are caused by cataracts, which is why a thorough assessment is essential before deciding on treatment.
When is cataract surgery recommended?
Cataracts are not treated based on how they look, but on how they affect your vision and daily activities. Surgery is usually recommended when cataracts begin to interfere with tasks such as driving, reading, working, or maintaining independence.
There is no benefit in waiting until a cataract becomes “fully mature.” Modern cataract surgery in Dubai and across the UAE is typically performed when symptoms become bothersome and impact quality of life.
Understanding cataract surgery
Cataract surgery involves removing the cloudy natural lens and replacing it with a clear artificial lens, known as an intraocular lens (IOL). This lens remains in place permanently and does not require maintenance.
Cataract surgery is one of the most commonly performed and successful surgical procedures worldwide. Studies cited by the National Institutes of Health (NIH) show that over 95% of patients experience improved vision following cataract surgery, assuming there are no other underlying eye conditions.
The procedure is usually performed as a day surgery, under local anaesthesia, and typically takes less than 30 minutes per eye.
Life after cataract surgery
Most patients notice improved vision within days of surgery, with gradual refinement over the following weeks. Eye drops are prescribed for a short period to reduce inflammation and prevent infection.
During recovery, patients are advised to:
- Avoid rubbing the eyes
- Use prescribed eye drops as directed
- Wear sunglasses outdoors to protect from bright light
- Avoid heavy lifting or strenuous activity for a short period
At Moorfields Eye Hospital Dubai, patients receive personalised post-operative care and follow-up to ensure smooth recovery and optimal visual outcomes.
Why early assessment matters
Left untreated, cataracts can eventually lead to significant vision impairment. Early assessment allows for:
- Timely planning of surgery
- Monitoring of progression
- Differentiation from other eye conditions
- Better surgical outcomes
With advances in surgical techniques and lens technology, cataract surgery today offers not only vision restoration but also the opportunity to improve overall visual quality for patients across Dubai and the UAE.
Summary
Cataracts are a common age-related eye condition that can gradually affect vision and quality of life. While cataracts cannot be reversed with medication, cataract surgery is a safe and effective treatment that restores clarity and visual function for millions of people each year.
If you notice changes in your vision, a comprehensive eye examination is the first step toward understanding the cause and exploring appropriate treatment options.
Frequently Asked Questions (FAQs)
1. Are cataracts preventable?
Cataracts are largely a natural part of ageing and cannot be completely prevented. However, certain lifestyle choices may help slow their development or progression. Protecting your eyes from excessive ultraviolet (UV) exposure by wearing sunglasses, maintaining good control of conditions such as diabetes, avoiding smoking, and following a healthy diet may all support long-term eye health. Regular eye examinations are also important, as they allow cataracts to be detected and monitored early.
2. Can cataracts affect both eyes at the same time?
Yes, cataracts commonly develop in both eyes. However, they often progress at different rates, meaning one eye may be affected earlier or more severely than the other. This difference can sometimes make the vision imbalance more noticeable. Each eye is assessed individually, and treatment decisions are based on how cataracts affect daily activities and vision in each eye.
3. Is cataract surgery painful?
Cataract surgery is generally not painful. It is usually performed under local anaesthesia, which numbs the eye and keeps you comfortable throughout the procedure. You may feel mild pressure or awareness, but pain is uncommon. After surgery, some patients experience mild irritation or grittiness, which typically settles within a short period and is well managed with prescribed eye drops.
4. How long does cataract surgery recovery take?
Recovery after cataract surgery is usually straightforward. Many people notice clearer vision within a few days, although vision may continue to improve gradually over several weeks. Most daily activities can be resumed relatively quickly, with certain precautions advised during the early healing period. Your ophthalmologist will guide you on activity levels and follow-up care to support a smooth recovery.
5. Will I still need glasses after cataract surgery?
This depends on the type of intraocular lens (IOL) implanted and your individual visual needs. Some lenses are designed to correct distance vision, while others may reduce the need for glasses for both near and distance tasks. Even with advanced lens options, some people may still require glasses for specific activities, such as reading or driving at night. Your surgeon will discuss suitable lens choices before surgery.
6. Can cataracts return after surgery?
Once a cataract has been removed, it cannot return. However, some patients may develop clouding of the thin membrane that holds the artificial lens in place, a condition sometimes referred to as “secondary cataract.” This is not a recurrence of the cataract and can be easily treated with a quick, painless laser procedure that restores clear vision.
7. Is cataract surgery safe for older adults?
Yes. Cataract surgery is commonly performed in older adults and is considered safe and effective. Age alone is not a limiting factor. What matters more is overall health, eye condition, and suitability for surgery. Many older patients experience significant improvements in vision, independence, and quality of life following cataract surgery.
8. Can cataracts cause complete blindness if untreated?
If cataracts are left untreated for a long time, they can lead to severe vision impairment and, in rare cases, functional blindness. However, in settings where regular eye care is accessible, this outcome is uncommon. Early detection and timely treatment help prevent cataracts from progressing to a stage where they significantly limit vision or daily functioning.
This blog on glaucoma awarness month has been contributed Dr. Salman Waqar, Consultant Ophthalmologist in Cataract and Glaucoma Surgery.
Glaucoma occurs when there is high pressure in the eye, which can lead to reduction or loss of vision due to damage to the optic nerve (the nerve that transmits signals from our eye to the brain). It is one of the leading causes of blindness worldwide, with nearly 60 million people already affected. This number is projected to increase by almost fifty percent over the next ten years.
January is Glaucoma Awareness Month and is an opportunity for us all worldwide to highlight this blinding condition (also known as the “silent thief of sight”).
Early detection and prompt treatment are essential. The campaign aims to increase awareness of the importance of annual eye examinations to diagnose and treat the condition early before vision is harmed for our loved ones and us.
Typically, your eye specialist will conduct the following very specialised and precise tests to screen for glaucoma:
- Eye pressure check
- Clinical evaluation of the optic nerve
- Visual Field testing
- Optical Coherence Tomography (OCT) scan of the nerves
If a diagnosis of glaucoma is made, treatment can be done with easy-to-use eye drops, gentle lasers or, in more advanced cases, with the latest surgical techniques. However, the treatment decision can vary from person to person, and your eye specialist will recommend a bespoke treatment plan keeping in mind your individual requirements.
For more information, please visit www.glaucoma.org”
This blog on Neuro-ophthalmology has been contributed by Dr. Salma Yassine, Consultant Ophthalmologist in Paediatric & Neuro-ophthalmology
What is neuro-ophthalmology?
Neuro-ophthalmology is an ophthalmic subspecialty that addresses the relationship between the eye and the brain. The optic nerve acts as a cable that connects what we see through our eyes to the brain. The brain then changes the visual signals into images and helps us know what we are seeing. If the optic nerve is damaged, these visual signals are impaired, which leads to decreased visual perception. The field of neuro-ophthalmology deals with such neurological conditions that affect the eye and causes problems with vision. Some neuro-ophthalmic disorders can cause permanent damage if not diagnosed and treated adequately.
What are the most common symptoms of neuro-ophthalmic diseases?
Some common Neuro-ophthalmology symptoms include reduced vision, double vision, headaches, impaired colour vision, and visual field cuts. These symptoms are not to be ignored, if you face any of them, you must immediately seek advice from a neuro-ophthalmologist
What are common types of neuro-ophthalmic diseases?
A few of the most common neuro-ophthalmic conditions are optic neuritis, ischemic optic neuropathy, comprehensive optic neuropathy (pituitary tumours), papilledema, inflammatory and infectious optic neuropathies, cerebrovascular disorders involving vision, tumours involving vision, blepharospasm and hemifacial spasm, nystagmus, thyroid eye disease, myasthenia gravis, ocular motor disorders, pupillary abnormalities, hereditary optic neuropathies in patients who have unexplained vision loss
Some disorders that require immediate attention from neuro-ophthalmologists include;-
- Optic neuritis: It is an eye disorder that is caused by inflammation of the optic nerves. This inflammation can be caused by infection or autoimmune disorders like multiple sclerosis and neuromyelitis optica. It is a disease that usually affects young adults in 1 eye but often affects 2 in children. Patients with optic neuritis can develop nagging eye pain, pain with eye movements, blurry vision, and loss of colour perception. These issues can be serious because it can lead to permanent vision loss.
- Papilledema : It is a condition in which optic nerves swell up due to increased intracranial pressure. It is often accompanied by headaches, dimming of vision and rushing noises in the ears. Papilledema can lead to optic atrophy and blindness if not treated in a timely manner. Sometimes papilledema can be a warning sign for a tumour or haemorrhage. If papilledema is not traced to a particular problem, then it is called idiopathic cranial hypertension.
- Nutritional optic neuropathy: Toxic substances found in alcohol and tobacco can also damage the optic nerve. Certain vitamin deficiencies like folic acid and vitamin B complex can cause optic neuropathy
- None ischemic arthritic optic neuropathy (NAION): There are many risk factors for NAION, some of which include uncontrolled sugar levels in diabetics or high blood pressure in hypertensive patients. These systemic conditions can affect the blood vessels that supply the optic nerve, which can result in disabling vision loss.
- Strabismus (squints): It is a disorder when both eyes cannot align in one direction, which can cause double vision. Paralytic strabismus occurs when the muscles are unable to move the eye, disrupting the coordination between both eyes. This could be due to a lesion compressing the nerves that connect to the ocular muscles or due to microvascular damage to these nerves
This blog on Dry eyes has been contributed by Dr. Alia Issa, Aesthetic Oculoplastic Surgeon at Moorfields Eye Hospital Dubai
Dry eye disease is one of the most common reasons people seek advice from an ophthalmologist. While it is often a minor irritation, dry eye can significantly affect comfort, vision, productivity, and overall quality of life. In a city like Dubai, where air conditioning, screen use, and environmental factors are part of everyday life, dry eye symptoms are particularly prevalent.
It is therefore essential to understand its causes, symptoms, and treatment options to effectively manage it.
What is Dry Eye Disease?
Dry eye disease occurs when the surface of the eye does not receive adequate lubrication. This may be due to reduced tear production, increased tear evaporation, or an imbalance in the quality of the tear film. Tears play an important role in maintaining eye comfort, clear vision, and protection against infection. When the tear film is unstable, the surface becomes irritated and inflamed, and, over time, this irritation can create a cycle in which dryness leads to inflammation, and inflammation further worsens tear quality.
Why is Dry Eye Disease common in Dubai and the UAE?
Environmental and lifestyle factors play a major role in the development and worsening of dry eye symptoms. Studies in the United Arab Emirates have shown that dry eye disease affects a large proportion of people, with one cross-sectional study in Dubai estimating that about 62.6% of adults report dry eye symptoms.
Common causes of Dry eye disease include:
- Air conditioning, which reduces humidity and increases tear evaporation
- Hot, dusty, and polluted environments, which irritate the ocular surface
- Prolonged digital screen use, leading to reduced blinking
- Contact lens wear, especially for extended hours
- Exposure to cigarette smoke
What are the common symptoms of Dry Eye Disease?
Dry eye symptoms can vary in severity and may fluctuate throughout the day. In the UAE, symptoms may also fluctuate throughout the year, often worsening during the hotter months when air conditioning use increases and outdoor conditions are more challenging for the eyes.
Common symptoms include:
- A gritty or foreign body sensation
- Burning, stinging, or soreness
- Redness of the eyes
- Excessive tearing (a reflex response to dryness)
- Blurred or fluctuating vision
- Eye fatigue, especially after screen use
Because symptoms can be subtle or inconsistent, dry eye is sometimes overlooked or self-treated for long periods before a proper diagnosis is made. Some people experience significant discomfort despite minimal visible signs, while others may have advanced disease with surprisingly mild symptoms.
Who is at risk of Dry Eye Disease?
Dry eye disease can affect people of all ages, but certain factors increase the likelihood of developing symptoms. You may be at higher risk if you:
- Spend long hours using digital screens, such as computers, tablets, or smartphones
- Work or live in air-conditioned environments for much of the day
- Are over the age of 40, as tear production and tear quality tend to reduce with age
- Are a woman, as hormonal changes can contribute to a higher risk of dry eye
- Wear contact lenses, particularly for extended periods
- Live in hot, dry, dusty, or polluted environments, such as those common in the UAE
- Have underlying medical conditions, including autoimmune or thyroid disorders
- Take certain medications, such as antihistamines, antidepressants, or blood pressure treatments
- Have had previous eye surgery, which can temporarily or permanently affect tear stability
What are the Different types of Dry Eye Disease?
Not all dry eyes are the same, and when diagnosing dry eye disease, ophthalmologists differentiate between two main types, although many people experience a combination of both.
- Evaporative Dry Eye: The most common form of dry eye. It occurs when tears evaporate too quickly from the eye’s surface, often due to dysfunction of the meibomian glands in the eyelids. These glands produce the oily layer of the tear film, which slows evaporation.
- Aqueous-Deficient Dry Eye: This type occurs when the lacrimal glands do not produce enough tears. It is more commonly associated with autoimmune conditions, ageing, or certain medications.
Because these types have different underlying causes, they require different treatment strategies. This is why a detailed assessment is essential before recommending treatment.
How is Dry Eye Disease diagnosed?
Dry eye disease cannot be accurately diagnosed based solely on symptoms. A comprehensive evaluation typically includes:
- A detailed medical and lifestyle history
- Slit lamp examination of the eyelids and ocular surface
- Assessment of tear quantity and quality
- Evaluation of the meibomian glands
- Specialised tests to assess tear film stability
A specialist dry eye assessment allows all contributing factors to be identified, which is essential because dry eye disease is rarely caused by a single issue and often involves several overlapping factors.
How is Dry Eye Disease treated?
Dry eye disease is a chronic condition, and successful management usually involves addressing both symptoms and underlying causes. Chronic does not mean constant and many individuals experience significant improvement and long periods of comfort once the right treatment combination is found.
Treatment plans vary depending on the type and severity of dry eye and may include:
Lifestyle and Environmental Adjustments
- Improving blinking habits and following the 20-20-20 rule
- Reducing direct exposure to air conditioning or fans
- Using humidifiers where appropriate
Artificial Tears and Lubricants
Different formulations are used depending on whether lubrication, oil replacement, or inflammation control is needed. Not all eye drops are the same, and choosing the right type is important for effective relief.
Eyelid Hygiene and Warm Compresses
These help improve meibomian gland function and tear film stability.
Specialised treatment
For some individuals, dry eye symptoms persist despite lifestyle adjustments and regular use of eye drops. In these cases, more specialised treatments may be recommended following a detailed assessment by a dry eye specialist.
At Moorfields Eye Hospital Dubai, a range of specialised dry eye treatments are available, depending on the underlying cause and severity of the condition. These may include:
- Prescription medications, used in selected cases to help reduce inflammation or support tear quality
- Tear duct (punctal) plugs, which help retain natural tears on the eye surface by reducing tear drainage
- Intense Pulsed Light (IPL), an advanced in-office treatment that may be recommended for certain forms of evaporative dry eye, particularly when related to meibomian gland dysfunction
- Lipiflow, an in-office treatment for dry eyes that gently warms and massages the eyelids to unblock the meibomian glands, restoring the natural oil layer of the tear film and improving eye comfort.
- Treatment plans are customised to each patient, recognising that dry eye disease often involves multiple contributing factors and that management is rarely a one-size-fits-all approach.
Why is it important to manage Dry Eye Disease early?
If left untreated, dry eye disease can lead to chronic discomfort, inflammation, and damage to the ocular surface. It can also affect visual clarity, reading comfort, and work performance, particularly for individuals who spend long hours on digital devices. In more severe or prolonged cases, ongoing inflammation can compromise the eye surface and increase the risk of complications. Early assessment helps prevent this progression and reduces the need for more intensive treatments later.
With appropriate diagnoses and tailored treatment, most people experience significant improvement in comfort and quality of life.
Conclusion
Dry eye disease is common, complex, and often underestimated. Understanding that dry eye has many contributing factors, whether environmental, systemic, and lifestyle-related, is the first step towards effective management. With a thorough assessment and an individualised treatment plan, symptoms can be controlled, and long-term eye health protected.
FREQUENTLY ASKED QUESTIONS (FAQs)
Is dry eye a permanent condition?
Dry eye disease is often a long-term (chronic) condition, particularly when linked to age, hormonal changes, environmental factors, or underlying health issues. However, this does not mean symptoms must be constant or severe. With the right diagnosis and a personalised treatment plan, most people can achieve good symptom control and enjoy long periods of comfort. Ongoing care and regular reviews help adapt treatment as needs change over time.
Why do my eyes water if they are dry?
Watery eyes may seem contradictory, but excessive tearing is actually a common sign of dryness. When the eye surface becomes irritated, the tear glands produce a surge of reflex tears. These tears are mostly watery and lack the oils and proteins needed for proper lubrication. As a result, they do not remain on the eye long enough to relieve dryness and may instead overflow onto the cheeks.
Can screen use really make dry eye worse?
Yes. When using computers, tablets, or smartphones, people tend to blink less often and less completely. Blinking is essential for evenly distributing tears across the eye surface. Reduced blinking increases tear evaporation, leading to dryness, irritation, and blurred vision. This is particularly relevant for individuals who spend long hours on screens in air-conditioned environments, such as offices in Dubai.
Are artificial tears safe to use every day?
Most artificial tears, especially preservative-free formulations, are safe for regular and long-term use. Different products are designed to address different aspects of dry eye, such as lubrication, oil replacement, or inflammation control. Using the most appropriate formulation is important, which is why an ophthalmologist may recommend specific drops based on your type of dry eye and symptom pattern.
Does dry eye affect vision permanently?
Dry eye most commonly causes fluctuating or blurred vision that improves with blinking or lubrication. In most cases, vision changes are temporary. However, if severe dry eye is left untreated, chronic inflammation can damage the eye surface and, in rare cases, permanently affect vision. Early diagnosis and appropriate management greatly reduce this risk.
Can diet affect dry eye?
Diet can play a supportive role in managing dry eye symptoms. Omega-3 fatty acids, found in foods such as oily fish and flaxseed, may help improve tear film quality in some individuals. Adequate hydration is also important, as dehydration can worsen dryness. While dietary changes alone may not resolve dry eye, they can complement medical treatments.
When should I see a specialist for dry eye?
If symptoms persist despite using over-the-counter eye drops, interfere with daily activities, or worsen over time, it is advisable to seek professional assessment. A specialist can identify the underlying causes of your dry eye and recommend targeted treatment rather than relying on trial-and-error solutions.
This blog has been authored by Dr. Salman Waqar, Consultant Ophthalmologist in Cataract and Glaucoma Surgery, who was the first in Dubai to insert the PAUL Implants in adults and children.
Glaucoma affects a significant percentage of the population worldwide, and the risk increases with age. The non-surgical treatment options available for most patients are medications to reduce pressure in the eye and laser trabeculoplasty, which targets the drainage angle of the eye.
However, for many patients with advanced glaucoma or complex secondary glaucoma, medications and laser treatments alone are not sufficient to control eye pressure and preserve vision.
In these circumstances, aqueous tube shunts (also known as aqueous shunt devices or glaucoma drainage devices) have a much broader range of efficacy even in patients with the highest risk.
The devices in common use are the Ahmed Valve and the Baerveldt Tube.
Now, at Moorfields Eye Hospitals UAE, we also offer surgery with the latest device known as the PAUL implant.
What is the PAUL implant?
The PAUL implant is the latest generation of aqueous shunt devices. It has been designed to optimize efficacy with a higher safety profile. It is composed of a soft tube that is inserted into the eye and drains away excess fluid thereby controlling the eye pressure. The diameter of this tube is less than half a millimeter and this prevents complications such as low pressure or corneal damage. The tube is connected to a thin and soft end-plate which is placed under the skin of the eye. This end-plate is very comfortable and causes no erosion or discomfort. It also does not degrade and lasts for the duration of the patient’s lifetime.
How does it work?
Glaucoma is most commonly associated with a build-up of fluid pressure inside the eye. This build-up of fluid pressure is caused by partial blockage of the natural drainage channel of the eye. This pressure can damage the optic nerve which carries images from the eye to the brain affecting your vision. This fluid produced inside your eye is called aqueous humour, which is different from your tears. The PAUL implant drains fluid from inside the eye to an end-plate on the outside, which is placed under a thin skin-like membrane covering the white of the eye called the conjunctiva. The fluid is then absorbed into the bloodstream.
What are the benefits?
The PAUL implant will lower your eye pressure and prevent further damage to the optic nerve caused by eye pressure (intraocular pressure). Its design ensures less chance of complications such as low IOP (hypotony), corneal damage and tube erosion, and a more predictable eye pressure control from the very first day after the surgery.
Are there any alternatives?
The closest alternatives to the PAUL implant are the traditional aqueous shunt implants such as the Baerveldt or Ahmed Implants. We aim to always individualise treatment options to your unique needs and will suggest the PAUL implant to you only if we feel it offers the best chance of controlling your eye pressure compared to other techniques.
This blog has been contributed Dr. Fahd Quhill, Consultant Ophthalmologist in Medical Retina and Ocular inflammatory disease
Panretinal laser photocoagulation is gold standard for treating proliferative diabetic retinopathy; it is still the only available treatment that will provide a diabetic patient with long term regression of their diabetic changes and prevent further vision impairment.
What does laser treatment involve?
Dilating drops will be instilled on the day, to dilate your pupils with additional drops given by the nurse to numb the surface of the eye. Then the doctor will position you at the laser, whereby a contact lens will be placed on the front of the eye to keep the eyelids open and to allow the doctor to visualize the back of the eye and apply the required laser beams accordingly. It is important you keep still during the procedure and listen carefully and follow the instructions given by the doctor. It normally takes 10 to 20 minutes to complete a laser treatment, all dependent on the type of laser and number of laser burns the doctor needs to apply.
Is laser painful?
Some patient do feel some discomfort; it is normally a pricking sensation that they can perceive when certain areas of the retina are treated.
How long will it take my vision to recover?
Normally immediately after the laser, your vision will be dark, this is normal and not a cause for concern; it is due to the back of the eye being exposed to the light. Within a few minutes it will clear, but it will take up to 24 hours for your vision to return to its previous level where you will be able to resume your normal daily activities.
You may experience mild eye ache after laser, and there is no harm in taking mild painkillers to help with the discomfort.
You also may notice a few floaters within the vision, which do eventually improve and settle with time.
What are the side effects of panretinal laser photocoagulation for diabetic retinopathy?
Well for effective treatment, we need treat to the peripheral areas of the retina to regress the abnormal changes and stabiles vision. But within the peripheral retina, the cells that are important for your peripheral vision and night vision reside. So you may notice a reduction in your night vision, and perceive changes within the peripheral field, often this settles with time and you quickly adapt. However these side effects commonly occur in patients who have received multiple laser treatments for diabetic retinopathy.
Also occasionally if you have pre-existing diabetic maculopathy, leakage or swelling at the central vision, panretinal laser can worsen these changes leading to blurred vision. Often this is self-limiting and it will spontaneously resolve, but occasionally intravitreal injections into the eye are required to reduce leakage and rehabilitate your vision.
Don’t forget?
We cannot always guarantee stabilsation and regression of your diabetic changes with a single laser treatment, often patients will require multiple laser treatments to achieve this goal. Or patients ocular condition needs intravitreal injections to be combined with retinal laser for the best results and visual outcome.
This blog has been contributed Dr. Salman Waqar , Consultant in Ophthalmologist in Cataract and Glaucoma Surgery.
Glaucoma occurs when the pressure in our eye becomes high leading to damage to the optic nerve (nerve that connects our eye to the brain and helps us see). It is important to lower the eye pressure urgently to protect the nerve.
This can be done with eye drops, lasers and surgical techniques. Usually eye drops and lasers are used as first line treatment, but if these are not effective we have to intervene surgically.
What is the Presserflo MicroShunt?
The MicroShunt is an 8 millimetre long tube that is inserted into the eye to help lower eye pressure in glaucoma and reduce the need for medication. It is made entirely of a synthetic and biocompatible material called SIBS.
The MicroShunt won’t be rejected by the body and will not disappear or disintegrate with time. As it is not metallic, it will not set off airport scanners and is safe if you need to have an MRI or CT scan.
How does it work?
Glaucoma is most commonly associated with a build-up of fluid pressure inside the eye. This build-up of fluid pressure is caused by partial blockage of the natural drainage channel of the eye. This pressure can damage the optic nerve which carries images from the eye to the brain affecting your vision. This fluid produced inside your eye is called aqueous humour, which is different from your tears. Like trabeculectomy surgery, the MicroShunt drains fluid from inside the eye to outside, under a thin skin-like membrane covering the white of the eye called conjunctiva. The fluid is drained and pooled under conjunctiva forming what is called a bleb.
What are the benefits?
The MicroShunt will lower your eye pressure and prevent further damage to the optic nerve caused by eye pressure (intraocular pressure).
Compared to other glaucoma procedures such as a trabeculectomy, MicroShunt has the advantage that the procedure is shorter, less invasive, and requires fewer post-operative visits. In addition, the drainage bleb created by the MicroShunt is usually less obvious than after a trabeculectomy and contact lens wearers are often still able to continue contact lens wear afterwards.
Are there any alternatives?
The closest alternatives to the MicroShunt will be a traditional trabeculectomy or aqueous shunt implant (Baerveldt, Ahmed or Paul Glaucoma Implant). We aim to always individualise treatment options to your unique needs and will suggest the MicroShunt to you only if we feel it offers the best chance of controlling your eye pressure using a minimally invasive approach.
Whilst sun exposure is an excellent source of vitamin D, not taking the necessary protective measures during the summer can have damaging effects on the eyes. Spending a lot of time under direct sun light and heat may accelerate the aging process of the eyes and lead to conditions such as cataracts and macular degeneration.
With temperatures reaching as high as 48°C in the UAE, our eyes are at risk of developing corneal burns, also known as photokeratitis. Therefore, it is extremely important to take the necessary precautions while enjoying summer activities in the sun.
Our Ophthalmologists share six effective tips to protect your eyes in the summer.
- Wear sunglasses with full UV protection – Increased exposure to UV radiation can damage the macula, a central part of the retina at the back of the eye, which gives us the ability to have the perfect, colored vision. UV radiation may also harm the front part of the eye (cornea and lens) leading to cataracts (clouding of lens), macular degeneration, pterygium (benign growth on the white of the eye) and corneal sunburn, which is painful and might cause temporary vision loss. Thus, medical grade tinted glasses that can block up to 100% of the sun’s UV radiations are essential for protecting your eyes in the summer.
- Lubricate your eyes – High temperatures and dry winds outdoors can lead to increased dry eye. Air conditioning use increases during summer which also leads to dry eye symptoms worsening. The best and most immediate way to address eye dryness is by using artificial tears to keep the eyes moist and refreshed.
- Nourish your body with antioxidants – Constant exposure to the sun’s rays can produce free radicals, roaming atoms in the body that can oxidize and damage the retina. Hence, consuming a diet that is rich in antioxidants will help cancel out the effects of free radicals. Antioxidants such as Lutein, zeaxanthin, and vitamins C can be found in oranges, berries and leafy vegetables and can be easily integrated into your diet.
- Stay hydrated – In general, drinking water is extremely important to maintain healthy functioning organs. Considering that the summer heat can make us lose more water through sweat, we need to drink more water to compensate for this loss. Also, if you drink diuretics such as coffee, consider drinking at least 2 litres of water per day. Dehydration is a leading cause of dry eye and irritation, so it is imperative to maintain balanced hydration levels during the summer months.
- Always wear swimming goggles – summer is synonymous with swimming. If you enjoy swimming, consider investing in goggles to protect your eyes. Pools are often disinfected with harsh sanitizers such as chlorine. Thus, using goggles can protect your eyes from coming in contact with potent sanitizers and reduce the likelihood of contracting an eye infection such as conjunctivitis, which leaves the surface of the eye red and dry.
- Avoid swimming with contacts – Another important precaution to take is to remove your contact lenses before swimming. In fact, swimming with contacts can have sight-threatening effects such as ulcers and infections. Additionally, pool or beach water is home to many microbes such as Acanthamoeba, which can result in infections in the eye and serious complications.
This blog has been contributed Dr. Alaa Bou Ghannam , Specialist in Neuro-Ophthalmology, Paediatric Ophthalmology & Glaucoma, and Adult Strabismus
Children have their own set of eye diseases that are at times different from what we see among adults. Below is a list of ten of the most common pediatric eye problems seen in a paediatric ophthalmologist’s clinic.
- Refractive errors: This is by far the most common paediatric eye condition. Usually, it is easily treated with glasses. It can be myopia, hyperopia or astigmatism. Children sometimes cannot verbalize their inability to see, so they might squint, blink, turn their heads or just give up on seeing all together which might affect their school performance.
- Strabismus: This happens when the eyes are not aligned together, with one or both eyes drifting or crossing. This can be congenital or acquired; it is usually treated with glasses or surgery. In some cases we can just observe but sometimes systemic workup is needed to rule out underlying conditions.
- Viral conjunctivitis: Eyes are red, watery and have purulent discharge. Typically, it involves one eye and then spreads to the other. Observation is usually the rule as most will resolve uneventfully within 4-10 days. It is highly contagious.
- Allergic conjunctivitis: Presents with itching, blinking, red and watery eyes. Typically involves both eyes simultaneously. It can be seasonal or related to a specific allergen. Severe condition is called vernal catarrh. Treatments include lubrication, antihistamine drops, steroids or cyclosporine drops in severe conditions.
- Amblyopia/ lazy eye: It happens when the brain favors one eye over the other, causing further decrease in vision in the weaker eye. This might be caused by a difference in refractive error between the two eyes, strabismus, or media opacification preventing clear images from reaching the retina. It must be treated early on with patching of the stronger eye or with atropine drops.
- Nasolacrimal duct obstruction: It is usually congenital. Infants have excessive tearing and discharge, treated with nasal massage to open up the nasolacrimal duct. Most resolve by the age of one.
- Chalazion/ stye: It is a benign growth on the eyelid caused by a blockage of the meibomian gland due to lid inflammation. Treatment is usually through lid massage. In most cases it resolves uneventfully. Sometimes, it gets infected and will need antibiotics. If it does not resolve in a month then incision and drainage is recommended.
- Congenital cataract: Infants are born with unilateral or bilateral opacification of the lens. Parents will see a white reflex in the pupils. It is recommended to remove the lens early on to prevent amblyopia.
- Congenital glaucoma: A condition where the pressure in the eye is elevated. Infants with glaucoma will have large eyes (buphthalmous) with tearing and light sensitivity. Surgery is the treatment of choice as drops might not be helpful.
- Retinoblastoma: It is a malignant cancer of the retina. Parents will notice a white reflex in the pupil. It needs urgent diagnosis and treatment that includes chemotherapy, laser therapy and/ or removal of the eyeball (enucleation).
Annual comprehensive eye examinations are recommended for all young children, as many eye conditions may be managed or treated more effectively with early screening and detection.
This blog on the importance of early diagnosis for glaucoma was authored by Dr. Salman Waqar, a Consultant Ophthalmologist in Cataract and Glaucoma Surgery.
Glaucoma is a term used to describe a group of conditions in which the eye pressure is high, leading to damage to the optic nerve (the nerve that connects our eye to the brain). This can lead to permanent damage to the field of vision. In severe cases can cause tunnel vision and blindness. Even in less severe forms, glaucoma can interfere with independent living and can even affect our ability to drive.
Prevention is the key. Regular eye exams with your eye specialist, particularly if there is a family history of glaucoma, can detect the condition early.
Fortunately, we now have many very sensitive tests that can diagnose the condition well before it causes any perceptible damage to your vision. These include Visual Field tests and Optical Coherence Tomography scans. Both are done in clinic and only take a few minutes with no discomfort.
Once the diagnosis is confirmed, the key is to lower the eye pressure and preserve vision. While searching for an eye care facility and a Glaucoma specialist, it’s best to look for a location that can offer the comprehensive treatment options shown below and an experienced Glaucoma Consultant, for long term relief and peace of mind.
What are the treatment options?
- Eye drops: There are a wide variety of eye drops which can be used to lower the eye pressure. They are usually taken once or twice a day but do need to be instilled regularly for the rest of your life.
- Lasers:
- Selective Laser Trabeculoplasty: This is a simple and painless laser treatment that only takes a few minutes to perform and you can go home the same day. It can be done either to supplement the effect of eye drops or to replace them completely. At the time of your consultation, your consultant will discuss how this can help you.
- Laser Peripheral Iridotomy: In a particular type of glaucoma (narrow angle glaucoma), a very small channel is created in the iris (the coloured part of your eye) using a special laser. This can not only help lower the pressure but can also prevent future attacks of very high pressure (called acute angle closure glaucoma)
- Cyclodiode: If the eye pressure is not being controlled despite best efforts with all other treatment options, this laser can be performed to stop production of fluid in the eye (this is done by a part of the eye called the ciliary body).
- Surgery: We am trained in all the latest surgical techniques for the treatment of glaucoma. These include:
- Cataract Surgery: For some, simply removing a developing cataract can not only lead to improvement in vision but can also lower the eye pressure.
- Cataract Surgery with iStent inject implantation: At the time of cataract surgery a very tiny titanium stent can be implanted into the eye which helps to drain fluid out of the eye thus lowering the pressure. This is part of an exciting new type of surgery called minimally invasive glaucoma surgery (MIGS).
- Cataract Surgery with goniosynechialysis: Sometimes an iStent cannot be safely placed as the drainage angle of the eye is narrow. In such circumstances the drainage area can be opened with a technique known as goniosynechialysis
- Trabeculectomy with antimetabolite injection: This involves creating a flap on the surface of the eye which allows fluid to drain out. A special anti-scarring medication is used to ensure success.
- Aqueous Shunt Devices: These devices comprise of a soft footplate connected to a plastic tube. The tube is inserted into the eye whilst the footplate is secured to the surface of the eye and drains fluid out. Performing either a trabeculectomy or aqueous shunt device insertion is reserved for cases that are not responding to other suitable treatments as listed above.
Early detection and prompt treatment of glaucoma is essential to preserve vision. An ongoing and strong support system surrounding you can make all the difference in living a fulfilling life despite glaucoma.
Choose a location and a doctor that consider individualised treatments to suit your personal needs. This will help you and your family understand and manage the condition whilst also maintaining your quality of life.