Selective Laser Trabeculoplasty (SLT) is a procedure used to reduce the pressure in the eye (also known as intra-ocular pressure). A laser beam is applied to the drainage channels, which helps to unclog them. This means the aqeous humour flows through the channels better, reducing the pressure in the eye. This is not a permanent… Continue reading Selective Laser Trabeculoplasty
Refractive Surgery
Most refractive errors can be corrected (or at least improved) by means of Refractive Surgery. This is a generic term, which comprises both Laser Refractive Surgery and correction by means of lens implants inside the eye. The latter is called Phakic intraocular lens (IOL) surgery. Most refractive errors can be corrected (or at least improved)… Continue reading Refractive Surgery
Presbyopia
Presbyopia is a vision condition which makes it difficult to focus on close objects. During middle age, usually beginning in the 40s, people experience blurred vision at near points, such as when reading, sewing or working at the computer. Presbyopia is a natural part of the ageing process of the eye. It is not a… Continue reading Presbyopia
What is Posterior Vitreous Detachment? Causes, Symptoms & Care
PVD is a common degenerative change, which affects one or both eyes in many people after middle age. It may present earlier in shortsighted patients or those who have sustained traumas to the eyes. Thickening of the jelly casts shadows on the retina and are seen as floating shapes. These black “floaters”in your vision move… Continue reading What is Posterior Vitreous Detachment? Causes, Symptoms & Care
Post-Operative Instructions
Following Retinal Surgery on leaving the hospital you are advised to have a quiet evening at home and to avoid strenuous exercise. For General Anaesthetic patients, as above and: Do not drive a vehicle Do not make any crucial financial decision Do not eat heavy meals or drink alcohol for 24 hours after being discharged
Paediatric Strabismus
Facts A squint is a condition where your eyes look in different directions. One eye turns inwards, outwards, upwards or downwards while the other eye looks forwards. The medical name for a squint is strabismus. The misalignment of the eyes can be caused by different factors. It can be an early developmental problem where the… Continue reading Paediatric Strabismus
Myopia
Myopia is a common refractive condition which causes individuals to be near-sighted: they see near objects clearly but distant objects are blurry. Myopia occurs when the cornea and lens focus the light in front of the retina instead of exactly on it. Symptoms of myopia include; difficulty seeing distant objects, squinting frequently, holding books or… Continue reading Myopia
Lacrimal Probing in Children
The tear duct is a channel/passage which runs from a tiny opening in the medial lids through the bone to the inside of the nose, and drains the tears and mucus the eye produces. It should open just before or just after birth but sometimes remains blocked for a considerable time after that, causing watering… Continue reading Lacrimal Probing in Children
Keratoconus
Keratoconus is a progressive thinning of the cornea. The cornea is the clear front window of the eye, which, along with the intra-ocular lens, focuses light on to the retina. The cornea normally is a smooth, round dome-shaped structure; however in keratoconus it becomes very thin and irregular and it starts to protrude from the… Continue reading Keratoconus
About Intravitreal Injection
The macula is the central part of the retina at the back of the eye. It is responsible for fine vision (reading, writing, watching television, and recognising faces). Patients with diabetes may develop macular oedema (swelling of the retina) due to leaking of fluid from blood vessels. This causes the vision to become blurred. A… Continue reading About Intravitreal Injection
Hypermetropia
A refractive condition of the eye in which vision is better for distant objects than for near objects. It can be called far sightedness or hypermetropia. Symptoms of Hypermetropia can include; blurred vision, asthenopia (eye strain), accommodative dysfunction, binocular dysfunction, amblyopia and strabismus. It results from the eyeball being smaller than average, causing images to… Continue reading Hypermetropia
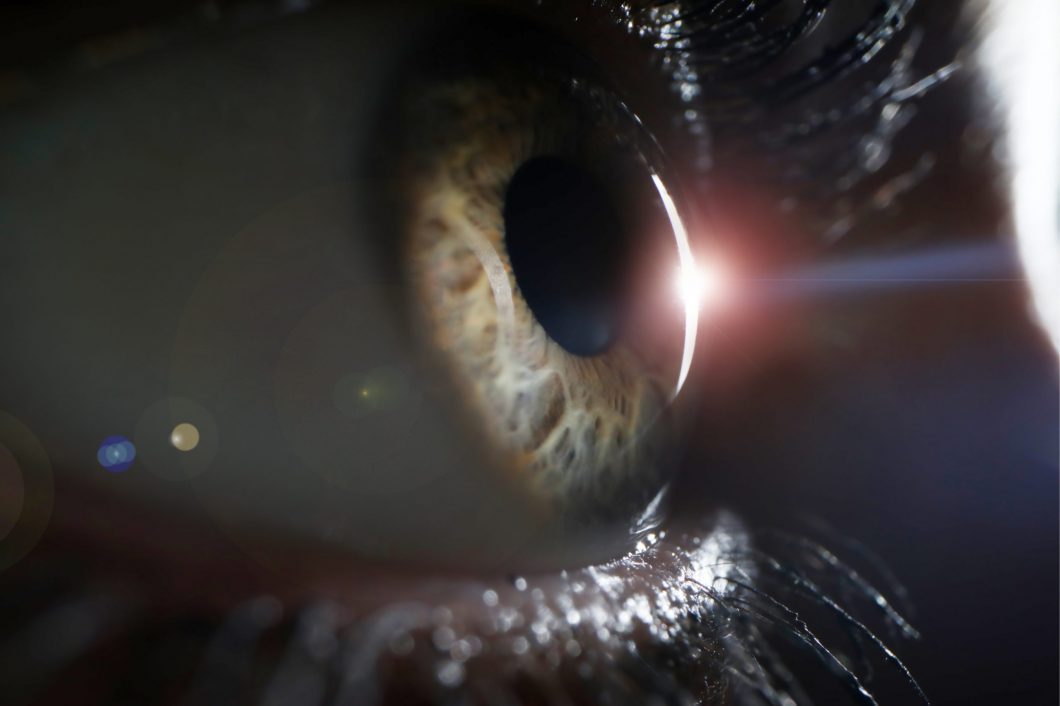
High Precision Refractive Surgery
When you decide on an eye laser treatment, you expect the best possible results. The more fully developed the methods are, the better the outcome will be. The SCHWIND AMARIS 750S offers you the leading technology for your laser treatment – superior in all important aspects: Speed, precision, safety and comfort.