Selective Laser Trabeculoplasty (SLT) is a procedure used to reduce the pressure in the eye (also known as intra-ocular pressure). A laser beam is applied to the drainage channels, which helps to unclog them. This means the aqeous humour flows through the channels better, reducing the pressure in the eye. This is not a permanent… Continue reading Selective Laser Trabeculoplasty
Refractive Surgery
Most refractive errors can be corrected (or at least improved) by means of Refractive Surgery. This is a generic term, which comprises both Laser Refractive Surgery and correction by means of lens implants inside the eye. The latter is called Phakic intraocular lens (IOL) surgery. Most refractive errors can be corrected (or at least improved)… Continue reading Refractive Surgery
Presbyopia
Presbyopia is a vision condition which makes it difficult to focus on close objects. During middle age, usually beginning in the 40s, people experience blurred vision at near points, such as when reading, sewing or working at the computer. Presbyopia is a natural part of the ageing process of the eye. It is not a… Continue reading Presbyopia
What is Posterior Vitreous Detachment? Causes, Symptoms & Care
PVD is a common degenerative change, which affects one or both eyes in many people after middle age. It may present earlier in shortsighted patients or those who have sustained traumas to the eyes. Thickening of the jelly casts shadows on the retina and are seen as floating shapes. These black “floaters”in your vision move… Continue reading What is Posterior Vitreous Detachment? Causes, Symptoms & Care
Post-Operative Instructions
Following Retinal Surgery on leaving the hospital you are advised to have a quiet evening at home and to avoid strenuous exercise. For General Anaesthetic patients, as above and: Do not drive a vehicle Do not make any crucial financial decision Do not eat heavy meals or drink alcohol for 24 hours after being discharged
Paediatric Strabismus
Facts A squint is a condition where your eyes look in different directions. One eye turns inwards, outwards, upwards or downwards while the other eye looks forwards. The medical name for a squint is strabismus. The misalignment of the eyes can be caused by different factors. It can be an early developmental problem where the… Continue reading Paediatric Strabismus
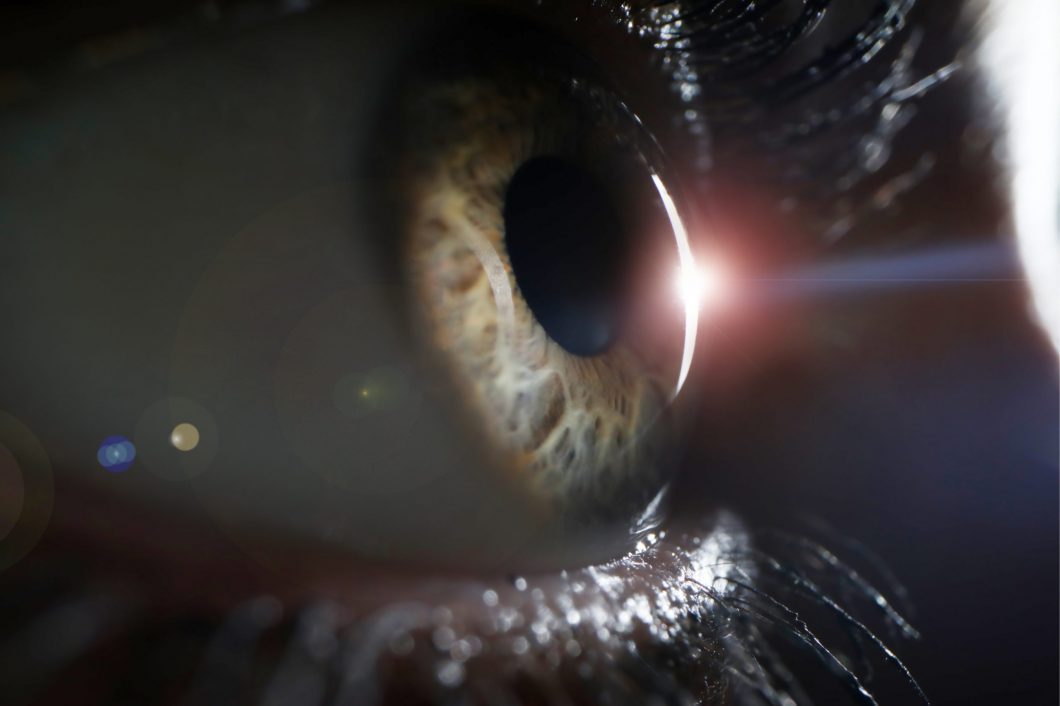
Keratoconus
Keratoconus is a progressive thinning of the cornea. The cornea is the clear front window of the eye, which, along with the intra-ocular lens, focuses light on to the retina. The cornea normally is a smooth, round dome-shaped structure; however in keratoconus it becomes very thin and irregular and it starts to protrude from the… Continue reading Keratoconus
Hypermetropia
A refractive condition of the eye in which vision is better for distant objects than for near objects. It can be called far sightedness or hypermetropia. Symptoms of Hypermetropia can include; blurred vision, asthenopia (eye strain), accommodative dysfunction, binocular dysfunction, amblyopia and strabismus. It results from the eyeball being smaller than average, causing images to… Continue reading Hypermetropia
Types of Diabetic Retinopathy
Introduction Diabetic retinopathy is a complication of diabetes and leads to high blood sugar, resulting in retinal disease, which can interfere with its ability to transmit images to the brain through the optic nerve. Blood vessels in the retina play an important role in supplying it with oxygen and nutrients, which keep it healthy and… Continue reading Types of Diabetic Retinopathy
Ocularist
[:en]An Ocularist makes and fits artificial eyes. Our aim at Moorfields Eye Hospital Dubai is to create a hand-crafted eye with a very natural look indistinguishable from the real eye. Made from acrylic, these artificial eyes are very strong, easy to maintain and are comfortable to wear. The Ocularist also provides a polishing and repair… Continue reading Ocularist
Ophthalmologist
[:en]Patients who need further specialist treatments for their eyes go to an Ophthalmologist. An Ophthalmologist is a medical doctor who specialises in the medical and surgical care of the eyes, visual system and in the prevention of eye diseases and injuries. They provide the full range of care including routine eye examinations, diagnosis and treatment… Continue reading Ophthalmologist
Orthoptist
[:en]Children who need to see an eye Specialist will initially go for a review with an Orthoptist – a health professional who specialises in eye movement problems and disorders that affect how the eyes work together. These conditions are typically diagnosed in childhood; so Orthoptists are highly experienced in examining children of all ages and… Continue reading Orthoptist