The central part of the retina (at the back of the eye) is called the macula and it has an important function as it controls the quality and sharpness of the central part of our vision.
Over time, the macular can wear out and lose some of its functionality which means loss of central vision (not the peripheral vision) and this can cause problems, when it comes to everyday tasks such as reading
The good news is that the deterioration of vision is usually happens quite slowly.
However, there are two types of macular degeneration – ‘wet’ and ‘dry’ – and what is known as the ‘wet’ form results in a sudden loss of central vision, which is a medical emergency and urgent treatment is needed.
Macula
The macula is a small, extremely important area at the centre of the retina, the light-sensing tissue at the back of the eye and is responsible for seeing fine details clearly.
With AMD (Age-related Macular Degeneration), you lose the ability to see fine details, close-up and at a distance.
AMD (Age-related Macular Degeneration)affects only your central vision and side and peripheral vision usually remains normal. For example, when people with AMD gradually lose the ability to recognise people’s faces.
Types of AMD (Age-related Macular Degeneration)
There are two types of AMD (Age-related Macular Degeneration).
Most people (about 75%) have a form called “early” or “dry” AMD, which develops when there is a build-up of waste material under the macula and thinning of the retina at the macula. Most people with this condition have near normal vision or milder sight loss in the initial stage.
10% of patients with dry AMD can progress to wet AMD. Wet AMD occurs when abnormal blood vessels grow underneath the retina and leak blood and fluid, which can prevent the retina from working properly.
Eventually the bleeding and scarring can lead to severe permanent loss of central vision, but the eye is not usually at risk of losing all vision (going ‘blind’) as peripheral vision remains. Symptoms of wet AMD include sudden central blurriness and distortion, where straight lines appear as wavy (metamorphopsia).
A late stage AMD is called geographic atrophy, where vision is lost through severe thinning or even loss of the macula tissue without any leaking blood vessels.
Treatments for AMD
Intravitreal injections (injections into the eye) for wet AMD use a medicine called anti-VEGF of which there are 2 licensed versions Eylea and Lucentis.
When anti-VEGF medicines are injected into the eye on a regular basis, it can stop the abnormal blood vessels growing, leaking and bleeding under the retina.
Most people with wet AMD need to have these injections several times a year, so patients need to get their care closer to home. Laser treatment is also available for specific forms of AMD, but is not effective for most cases.
There is currently no treatment for dry AMD.
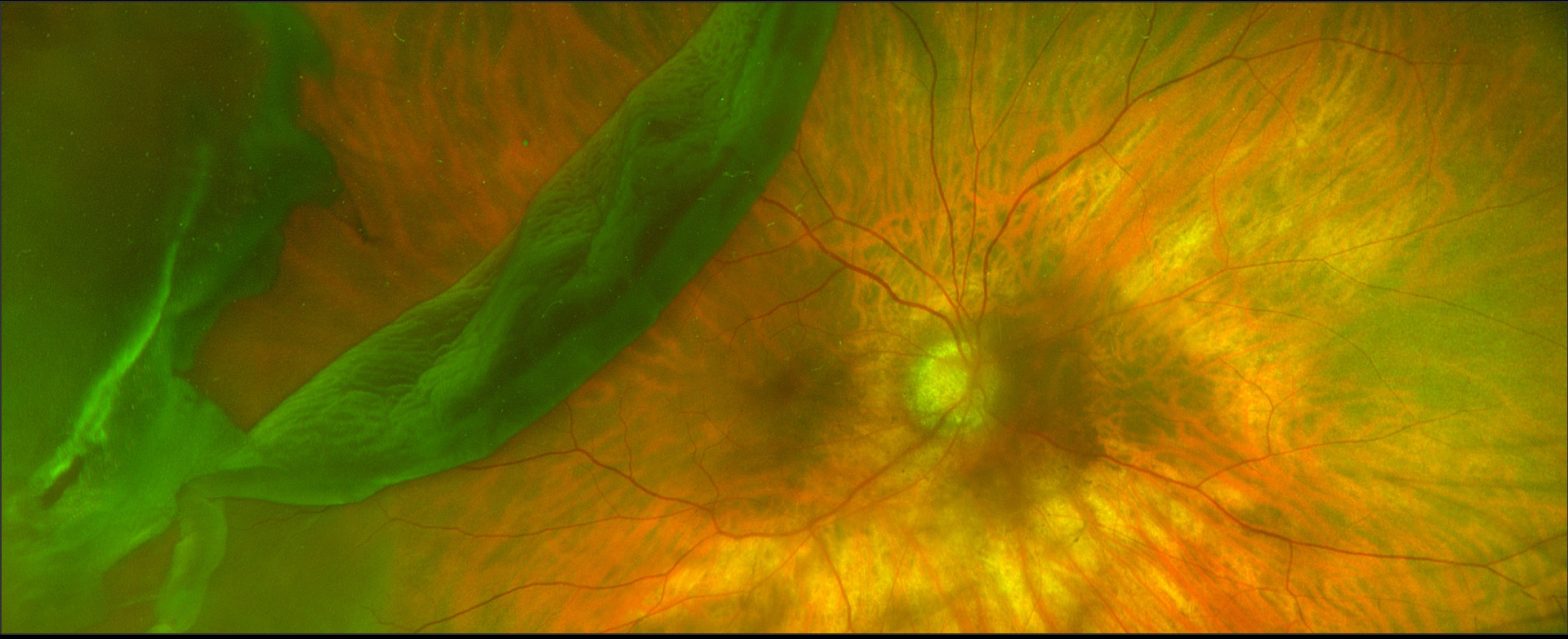
Retinal detachment is a condition when the thin lining at the back of the eye (the retina) begins to come away and separate itself from the underlying wall of the eye (the choroid) which contains blood vessels that supply it with vital oxygen and nutrients.
If not treated promptly, retinal detachment will lead to blindness in the affected eye.
A retinal detachment is usually caused by a tear in the retina and this is termed a Rhegmatogenous retinal detachment. There are other types of retinal detachment namely Traction retinal detachment which is usually seen in advanced diabetic retinopathy and Exudative retinal detachment (usually seen in people with inflammation). It is the Rhegmatogenous retinal detachment which needs urgent surgery in most cases.
Symptoms
Most people experience advance symptoms of a possible retinal detachment before losing their sight, including:
- sudden appearance of floaters – black dots, specks or streaks that float across the field of vision (usually only one eye is affected)
- web effect of lots of small floaters – some people see a single large black floater in the shape of a fly
- sudden short flashes (no more than one second) of light in the affected eye
- seeing a dark shadow like a curtain falling down from the outer aspect of the field of vision in the affected eye
- blurring or distortion of vision
Without immediate treatment, the vision in the affected eye will start to deteriorate, creating the effect of a shadow or ‘black curtain’ spreading across the vision. If a person experiences a shadow in the vision then It is extremely important to consult an eye doctor immediately before the shadow spreads across the centre of the vision.
Retinal detachment usually only occurs in one eye, however if one eye is affected, there is a 1 in 10 chance that the retina in your other eye will also detach.
You should contact your eye doctor immediately if you get any of these warning signs.
Causes
The retina at the back of the eye sends signals to the brain, enabling us to see. Without a blood supply, the retina’s nerve cells die leading to loss of sight.
Retinal detachment is usually the result of the retina becoming thinner and weaker with age. This causes a tear in the retina and once a tear develops the retina can pull away from the underlying blood vessel wall (the choroid).
Very short-sighted people have the greatest risk of developing age-related retinal detachment (though the risk is still very small) because they are often born with a thinner than normal retina in the first place.
Previous eye surgery, such as cataract removal, may also make the retina more vulnerable to damage.
In some cases, a tear can develop if the eye is suddenly injured, such as by a blow to the face but this is less common.
Diagnosis
If the eye specialist (ophthalmologist) suspects a retinal detachment, an examination of the back of the eye will confirm it.
Retinal Detachment Treatment
Urgent Retinal Detachment treatment is essential to lower the risk of permanent vision loss. The Retinal Detachment treatment is mainly surgery and eye drops will not help.
Most but not all detached retinas can be successfully reattached through different types of surgery, followed by a few months of recovery when vision will be weak, affecting lifestyle activities such as driving.
Some people’s eyesight does not fully return after surgery and they have permanently reduced peripheral (side) or central vision. This can happen even if the retina is reattached successfully.
This risk is higher the longer the detachment was left untreated.
Who does it affect?
Retinal detachment is rare. For example, only one in every 10,000 people will develop it in any given year in the UK.
As retinal detachment is associated with ageing, most cases affect older adults aged between 60 and 70. Retinal detachment caused by an injury can affect people of any age, including children.
Contact Moorfields Dubai for Retinal Detachment treatment today.
What is Glaucoma?
Glaucoma is a condition in which the fluid which is produced by the eye – known as the aqueous humour – does not drain away normally and this results in increased pressure inside the eye. If this condition is not treated, it can lead to damage of the optic nerve which connects the eye to the brain and loss of vision.
Signs and Symptoms
Glaucoma does not present symptoms until late stages, when it can cause damage to your field of vision. It generally starts at the periphery of the field of vision and then leads to a gradual narrowing or tunneling of the vision. If treatment is delayed, these defects can severely affect your vision and can cause “tunnel vision”.
Importance of Early Diagnosis
Early treatment can prevent damage from occurring, however, any damage that occurs is permanent. Therefore it is very important to diagnose the condition early to maintain the maximum level of peripheral vision. Risk factors for Glaucoma include short sightedness, diabetes and people with a family history.
If there is a history of glaucoma in your immediate family then regular eye checks are essential. Ideally, everyone over the age of 40 should have an eye test for glaucoma.
Tests for Glaucoma
At Moorfields Eye Hospital Dubai we have the latest equipment for diagnosing and staging glaucoma.
Pressure Check
A local anaesthetic drop which lasts only for 10-20 minutes will be placed in both eyes, then a small instrument is placed gently against the eye. This will measure the pressure inside the eye. Alternatively the pressure may be checked using air. A small puff of air is blown into your eye, this is not painful and gives a quick and accurate measurement of the pressure.
Pachymetry
This measures the thickness of the cornea by means of an ultrasound probe. It has proven to be important in determining precisely the Intraocular pressure.
Treatment
The treatment for Glaucoma focuses on reducing the pressure inside the eye, by lowering the amount of fluid being produced or by improving the drainage of the fluid away from the eye.
The usual treatment
is with eye drops that best suit your case. If you are prescribed eye drops, they must be taken regularly and according to the prescribed doses.
In cases resistant to medical treatment, surgery may need to be performed.
Ask our staff for glaucoma screening and follow-up packages which conveniently include all the above tests.
General Examination
The examination includes looking directly at the optic nerve at the back of the eye for any signs of damage.
Visual Field Testing
The peripheral vision is tested to see whether there has been any loss of vision at the outer edge of the field of vision.
Optical Coherence
Detecting Glaucoma early, before symptoms are apparent, is important and Tomography helps achieve this and so reduces the risk of any damage to the optic nerve.
The diode laser is a highly concentrated beam of light, which can be used to target and treat a selected area. Sometimes, laser treatment is recommended in order to avoid or delay the need for more invasive surgery. The diode laser is used to produce very small burns in the ciliary body, which produces the watery fluid called aqueous humour, and is situated behind the iris (coloured part of your eye). The reduced production of aqueous humour causes the eye pressure to fall.
A vitrectomy surgery is microsurgery performed to remove the jelly and replace it by a saline solution, gas or a special type of silicone oil. The most common reasons for operating on the retina are retinal detachment, diabetes and scarring on the retina.
For more information about vitrectomy surgery in Dubai, contact us today.
The operation to control the pressure within your eye is called a Trabeculectomy (trab-ec-u-lec-tomy). A Trabeculectomy operationis recommended for patients whose glaucoma continues to progress despite using eye drops and/or having laser treatment.The goal of the Trabeculectomy surgery is to help lower and control the eye pressure. The eye pressure is known as intraocular pressure. If this remains high, then further irreversible loss of vision from glaucoma may occur. This operation will not improve your vision or cure glaucoma, but aims to prevent or slow down further visual loss from glaucoma damage.
This information aims to answer some of the questions you may have about squint surgery. The information does not cover everything as every patient and squint is different. Your surgeon will discuss your particular case with you. Please ask the clinical staff about anything you want to be made clear.
What are the aims of surgery?
- To improve the alignment of the eyes, to make the squint smaller in size.
- In some patients, to reduce or try to eliminate double vision or to protect or restore binocular vision.
- Occasionally to improve head posture.
What happens before the day of surgery?
A pre-assessment is performed in the weeks leading up to the operation date.
What happens on the day of surgery?
Squint surgery is nearly always a day case procedure. Squint surgery is a common eye operation. It involves weakening or strengthening or altering the action of one or more of the extraocular muscles which move the eye. The muscles may be recessed (to weaken), resected (to strengthen), their insertions moved (to alter their action) or less commonly altered in some other way (advanced, plicated, tucked, belly sutured permanently to the globe etc).
The muscles are sutured into their new positions. The operation is carried out under general anaesthetic. The operation usually takes up to 60 minutes depending on the number of muscles that need surgery. Parents can go down to the operating theatre with your child and stay until he/she is asleep but cannot come in to watch the surgery. Remember to discuss which eye(s) is/are being operated on and why.
What are the success rates?
Overall about 90% patients/parents perceive some improvement in the squint after surgery. However, there is some unpredictability in the procedure, so that the squint may not be completely corrected by the operation. Many patients require more than one operation in their lifetime. If the squint returns it may be in the same or in the opposite direction and may occur at any time. The operation does not change visual acuity or refractive error. More patching may be needed after the operation.
Does the surgery cure the need for glasses or a lazy eye?
No, the operation does not aim to change the vision or need for glasses.
What are the risks of the operation?
Parents can be informed that squint surgery is generally a safe procedure. However, as with any operation, complications can and do occur. Generally these are relatively minor but on rare occasions they may be serious.
-
Under and overcorrection
The original squint may still be present (undercorrection) or the squint direction may change over (overcorrection). Occasionally a different type of squint may occur. Some patients may require another operation.
-
Double vision
Double vision after surgery is normal and often settles in days or weeks. Some patients may continue to experience double vision on side gaze. Permanent primary position diplopia is very rare in children.
-
Allergy/stitches
Mild allergy to postop drops: itching/irritation/ redness/puffiness of the eyelids. It usually settles quickly when the drops are stopped. Infection or abscess around the stitches. Cyst or granuloma related to the wound or sutures: occasionally needs further surgery.
-
Redness
Can take up to 3 months to resolve, occasionally the eye remains discoloured (red, yellowish) permanently, particularly with repeated operations.
-
Scarring
Most of the scarring of the conjunctiva not noticeable by three months, but occasionally visible scars will remain, especially with repeat operations.
-
Lost or slipped muscle
Muscle may slip back from new position during the operation or shortly after, limiting eye movements. May require further surgery and not always possible to correct. The risk of slipped muscle requiring further surgery is about 1 in 1,000.
-
Scleral perforation
If suture passed too deep or thin sclera: may require antibiotic treatment and laser/cryo treatment. Can affect sight (via endophthalmitis, vitreous haemorrhage, retinal detachment). Risk is up to 2%.
-
Infection
Infection is a rare complication but the risk increases if drops are not instilled as directed and treatment not sought promptly. Significant infection is extremely rare but in the worst cases can cause loss of vision in the eye (endophthalmitis, orbital cellulitis).
-
Loss of Vision
Very rare, loss of vision in the eye being operated can occur. Risk of serious damage to the eye or vision is approximately 1 in 30,000.
-
Anterior segment ischaemia
The blood circulation to the front of the eye can rarely be reduced following surgery, producing a dilated pupil and blurred vision. This usually only occurs in patients who have had multiple surgeries. The risk is about 1 in 13,000 cases.
-
Anaesthetic risks
Unpredictable reactions occur in around 1 in 20,000 cases and death in around 1 in 100,000.
What will it be like after the operation?
Eye(s) will be swollen, red and sore and the vision may be blurry. Start the drops that evening, and painkillers suitable for age of the child, such as paracetamol and ibuprofen suspension, can be taken. The pain usually wears off within a few days. The redness and mild discomfort can last for up to 3 months particularly with repeat squint operations.
Care after the operation
- Use the eye drops as directed
- Attend your follow up appointment(s) to ensure the eye is healing well
- Use cooled boiled water and a clean tissue or cotton wool to clean any stickiness from the eyes
- Don’t rub the eye(s)
- No swimming for 4 weeks
- Continue using glasses if have them
- Your child will need a few days to one week off nursery or school.
This information aims to answer some of the questions you may have about squint surgery. However, it does not cover everything as every patient and squint is different. Your surgeon will discuss your particular case with you. Please ask the clinical staff about anything you want to be made clear.
What is the aim of surgery?
- To improve the alignment of the eyes, to make the squint smaller in size.
- In some patients, to reduce or try to eliminate double vision.
- Occasionally to improve an abnormal position of the head.
How is the surgery done?
Squint surgery is a very common eye operation. It usually involves tightening or moving one or more of the outside eye muscles which move the eye. These muscles are attached quite close to the front of the eye under the conjunctiva, the clear surface layer. The eye is never taken out of the socket during surgery. Stitches are used to attach the muscles in their new positions.
Squint surgery is nearly always a day case procedure so you should be in and out of hospital on the same day.
There are two kinds of squint operation – adjustable and non-adjustable:
Non adjustable surgery
The operation is usually carried out under general anaesthetic. The operation usually takes up to 60 minutes depending on the number of muscles that need surgery. When you have recovered from the anaesthetic and the nurses are happy for you to be discharged, you are free to go home – usually a few hours later.
Adjustable surgery
Squint surgery using an adjustable suture may give a better result in certain types of squint e.g. patients who have had a squint operation before, patients with a squint due to injury or patients with thyroid eye problems.
Part 1 – The main operation
The main part of the operation is carried out in the operating theatre usually under general anaesthetic (with you asleep).
Part 2 – Adjusting the stitch
Once you have woken up from the anesthetic the final position of the muscles is adjusted when you are awake and able to look at a target. This is particularly useful for treating double vision. If you wear glasses for distance or near, these will need to be brought in with you for this part of the operation. Adjustment is usually done on the ward, after drops of anaesthetic have been put into the eye to take away any pain. You may however feel a pressure sensation.
Before the day of surgery
A pre-assessment is performed in the weeks leading up to the operation date.
What happens on the day of surgery?
You will be asked to come early so that you can be prepared for surgery. You should not drink or eat before the operation: the exact timings of this will be given before the day of the operation. Before being discharged after the operation, you will receive eye drops with instructions and a follow up appointment.
Does the surgery cure the squint?
Overall about 90% patients feel some improvement in their squint after surgery. The amount of correction that is right for one patient may be too much or too little for another with exactly the same size squint, so that the squint may not be completely corrected by the operation. Although the eyes may be straight just after surgery, many patients require more than one operation in their lifetime. If the squint returns it may drift in either the same or opposite direction. We can’t predict when that drift may occur.
What are the risks of the operation?
Squint surgery is generally a safe procedure. However, as with any operation, complications can and do occur. Generally these are relatively minor but on rare occasions they may be serious.
-
Under and overcorrection
As the results of squint surgery are not completely predictable, the original squint may still be present (undercorrection) or the squint direction may change over (overcorrection). Occasionally a different type of squint may occur. These problems may require another operation.
-
Double vision
You may experience double vision after surgery, as your brain adjusts to the new position of the eyes. This is common and often settles in days or weeks but may take months to improve. Some patients may continue to experience double vision when they look to the side in order to achieve a good effect when the eyes look straight ahead. Rarely, double vision whilst looking straight ahead can be permanent in which case further treatment might be needed. If you already experience double vision, you might experience a different type of double vision after surgery. Botulinum toxin injections are sometimes performed before surgery to assess your risk of this.
-
Allergy/stitches
Some patients may have a mild allergic reaction to the medication they have been prescribed after surgery. This results in itching/irritation and some redness and puffiness of the eyelids. It usually settles very quickly when the drops are stopped. You may develop an infection or abscess around the stitches. This is more likely to occur if you go swimming within the first four weeks after surgery. A cyst can develop over the site of the stitches, which occasionally needs further surgery to remove it.
-
Redness
The redness in the eye can take as long as 3 months to go away. Occasionally the eye does not completely return to its normal colour, particularly with repeated operations.
-
Scarring
Most of the scarring of the conjunctiva (skin of the eye) is not noticeable by three months, but occasionally visible scars will remain, especially with repeat operations.
-
Lost or slipped muscle
Rarely one of the eye muscles may slip back from its new position during the operation or shortly afterwards. If this occurs, the eye is less able to move around and, if severe, further surgery can be required. Sometimes it is not possible to correct this. The risk of slipped muscle requiring further surgery is about 1 in 1,000.
-
Needle penetration
If the stitches are too deep or the white of the eye is thin, a small hole in the eye may occur, which may require antibiotic treatment and possibly some laser treatment to seal the puncture site. Depending on the location of the hole, the sight may be affected. The risk of the needle passing too deeply is about 2%.
-
Anterior segment ischaemia
The blood circulation to the front of the eye can very rarely be reduced following surgery, producing a dilated pupil and blurred vision. This usually only occurs in patients who have had multiple surgeries. The risk is about 1 in 13,000 cases.
-
Infection
Infection is a rare complication but the risk increases if drops are not instilled as directed and treatment not sought promptly. Significant infection is extremely rare but in the worst cases can cause loss of vision or the eye (endophthalmitis, orbital cellulitis).
-
Loss of vision
Although very rare, loss of vision in the eye being operated can occur from this surgery. Risk of serious damage to the eye or vision is approximately 1 in 30,000.
-
Anaesthetic risks
Anaesthetics are usually safe but there are small and potentially serious risks. Unpredictable reactions occur in around 1 in 20,000 cases and unfortunately death in around 1 in 100,000.
Remember: these complications are detailed for your information and that the vast majority of people have no significant problems. After the operation the eye(s) will be swollen, red and sore and the vision may be blurry. The eye may be quite painful.
Start the drops you have been prescribed that evening, and painkillers such as paracetamol and ibuprofen can be taken. The pain usually wears off within a few days. The redness and discomfort can last for up to 3 months particularly with adjustable and repeat squint operations.
You should not sign any legal documents or drive for 48 hours after the general anaesthetic.
We would advise that you may need one or occasionally two weeks off work. Work and normal activities including sport can be resumed as soon as you feel comfortable to do so. It is quite safe to use the eyes for visual tasks, for example reading, watching television. You should return for follow up as advised.
Summary of care after the operation
- Use the eye drops
- Use painkillers such as paracetamol and ibuprofen if the eyes are painful
- Use cooled boiled water and a clean tissue or cotton wool to clean any stickiness of the eyes and avoid water entering the eyes from the bath or shower for the first two weeks
- Don’t rub the eye(s) as this may loosen the stitches
- No swimming for 4 weeks
- Attend the postop clinic appointment
- Continue using glasses if you have them
- Avoid contact lens wear in the operated eye(s) until advised it is safe by the doctor or orthoptist
Selective Laser Trabeculoplasty (SLT) is a procedure used to reduce the pressure in the eye (also known as intra-ocular pressure). A laser beam is applied to the drainage channels, which helps to unclog them. This means the aqeous humour flows through the channels better, reducing the pressure in the eye. This is not a permanent treatment, and may need to be repeated in the future to control the eye pressures adequately. The procedure does not require admission to hospital and is carried out in the outpatients department.
Most refractive errors can be corrected (or at least improved) by means of Refractive Surgery. This is a generic term, which comprises both Laser Refractive Surgery and correction by means of lens implants inside the eye. The latter is called Phakic intraocular lens (IOL) surgery.
Most refractive errors can be corrected (or at least improved) by means of Refractive Surgery. This is a generic term, which comprises both Laser Refractive Surgery and correction by means of lens implants inside the eye.
Presbyopia is a vision condition which makes it difficult to focus on close objects. During middle age, usually beginning in the 40s, people experience blurred vision at near points, such as when reading, sewing or working at the computer.
Presbyopia is a natural part of the ageing process of the eye. It is not a disease, and it cannot be prevented. Presbyopia is diagnosed with a routine eye examination. Eyeglasses with bifocal or progressive addition lenses are the most common correction for presbyopia.
PVD is a common degenerative change, which affects one or both eyes in many people after middle age. It may present earlier in shortsighted patients or those who have sustained traumas to the eyes.
Thickening of the jelly casts shadows on the retina and are seen as floating shapes. These black “floaters”in your vision move with the eye and then settle as the eye rests. These are often described by patients as a “cobweb” or “insects”.
You may also be aware of flashing lights, like little flickers in the outer periphery. Usually these do not highlight a problem, however, it is important to have the eye thoroughly checked, as occasionally a retinal tear or a retinal detachment may occur.