Keratoconus and its Modern Treatments
This blog on ‘Keratoconus and modern treatments’ has been contributed Dr. Osama Giledi, Consultant Ophthalmologist, Specialist in Cornea, Cataract and Refractive vision correction surgery.
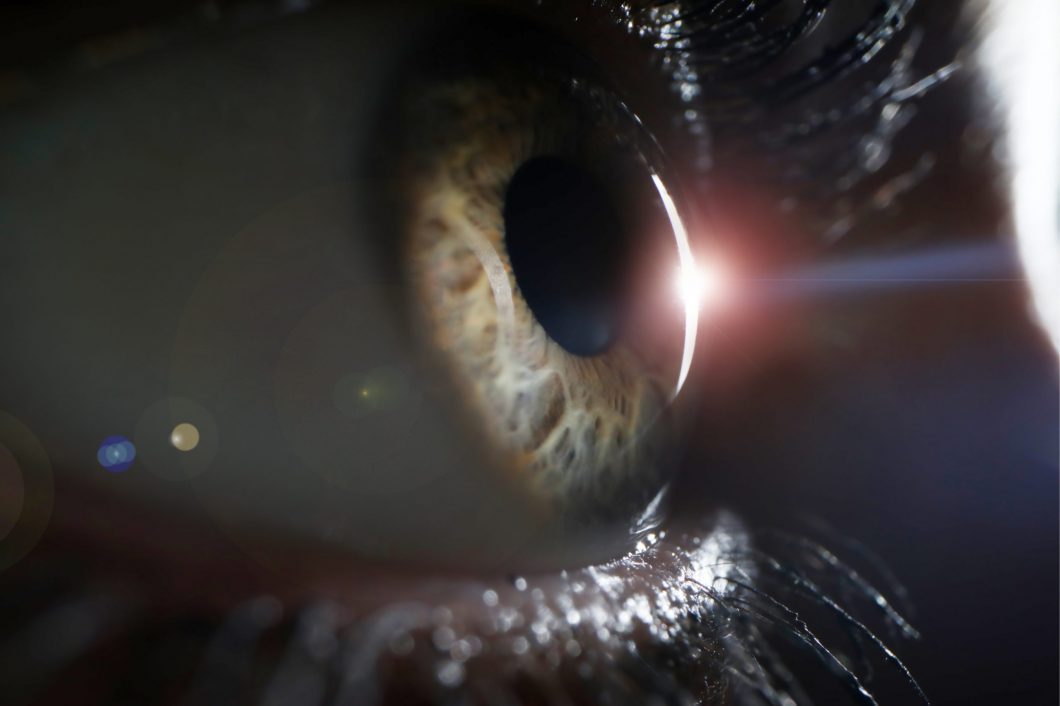
The cornea is the eye window which controls and focuses the entry of light into the eye, and in cases of keratoconus, there is a pathological decline in the thickness and rigidity of the cornea, which leads to irregular bulging of the cornea to a cone-like shape, which causes reduced vision from irregular astigmatism.
Corneal keratoconus usually affects both eyes and each eye may be affected differently, and usually occurs in people between the ages of 10 to 25 years. The condition may progress for 10 years or more and then slow down or stabilize. As the condition progresses, vision becomes distorted and blurred, with an increased sensitivity to light and glare.
Keratoconus presents itself in more certain ethnic groups, such as the Arab countries, southern Europe, and southern Asia. Environmental and genetic factors are potential causes, but the exact cause is uncertain.
Eye rubbing is a major risk factor. It is associated with some disease such as atopy and asthma. Also associated with some syndromes such as Down syndrome. If you have a family history of keratoconus, you have a greater chance of developing keratoconus. Pregnancy can make keratoconus progress more.
New corneal scans especially the 3 dimension scan such as pentacam help to diagnose Keratoconus at early stage.
Traditional treatment of keratconus was through glasses, hard contact lenses and corneal grafts. However, modern treatments for keratconus is used to stop the progress of Keratoconus, improve the shape of the cornea, and improve vision as well as avoiding the need for corneal graft.
Glasses or contact lenses can be used to correct nearsightedness and astigmatism in the early stages of keratoconus. As the Keratoconus progress, the patient needs a special solid contact lens.
Corneal collagen crosslinking
It is a procedure designed to halt the progression of keratoconus. The modern approach of accelerated pulsed crosslinking is used to ensure an easier procedure for the patient. We use ultraviolet A (UVA 360 nm), Riboflavin( vitamin B2) to stiffen and harden the cornea about four times and this stops the deterioration of keratoconus. The process is carried out under topical anesthesia and several drops of riboflavin are placed in the eye for about 15 minutes and activated by ultraviolet (UVA) rays for eight to thirty minutes. The corneal cross linakge is considered one of the safest and most successful operations used to stop keratoconus degradation and may lead to some improvement in some cases.
Intracorneal rings ( Ferrara, Kerarings or Intacus)
Intracorneal rings are plastic inserts that are implanted into the cornea to alter the shape of the cornea. It used to restore the regularity of the cornea again or at least reduce the irregularity; it will flatten the steepened section of a keratoconic cornea to achieve better unaided and better corrected vision. This often allows for a reduced prescription of spectacles and/or contact lenses and in some cases, satisfactory vision without glasses or contact lenses.
It is recommended to implant cornea rings in cases where the eyeglasses or contact lens are not able to clearly improve vision.
There ring can add strength to the cornea and it can be removed easily if it does not improve vision much.
The installation of rings using a femtosecond laser (intralase) added a new dimension to this type of operation. The process became safer and more effective and the femtosecond laser enabled the ophthalmologists to place these rings in the most accurate depth and diameter possible within the cornea with great accuracy and are way better than old Manual surgery. There are different sizes and thickness of rings depending on the shape of the keratoconus.
topography-guided laser surgery (TG-PRK).
Using topography guided eximer laser to improve the irregularity for the cornea surface in keratconus is a new method, where the patient who cannot tolerate contact lenses and has bad vision with glasses. The aim is to remove very little tissue so the patient can see clearly with glasses. There is a risk of weakening the cornea with this procedure, so we need to do a corneal cross linkage and minimize the amount of tissue removed by the eximer laser. Patient should be aware it is not to get rid of the glasses.
Implantable contact lens inside the eye.
It is used in patients with very high astigmatism and myopia who can see reasonably with glasses but the glass prescription are very high or has imbalance between the two eyes. These are placed inside the eye and have the ability to correct high degrees of short-sightedness and astigmatism. It is safe and effective procedure in selective patient, but the daily hard lens often provides for better vision than this lens as it corrects all the irregularity of the cornea.
Treatment with corneal cross linkage and intra corneal ring and topo guided laser all requires a minimum level of thickening of the cornea. Here the role of early diagnosis and treatment is highlighted, and that when the cornea becomes very thin these treatments become not possible, which makes corneal transplantation the only remaining treatment for such cases.
Corneal transplantation
It is recommended in advanced cases of keratoconus.
Out of all types of organ transplant surgeries (heart, lung, and kidney), corneal transplantation is the most widespread and successful of these.
We use modern ways to prepare the cut of both the donor and recipient cornea including using femtosecond laser.
There are various methods used for corneal transplant surgery. The old method includes removing the full thickness of diseased cornea and fixing the healthy cornea with stitches. As for following modern methods, the diseased frontal layers (DALK) is replaced and the patient retains the posterior portion of the cornea, thereby reducing the percentage of corneal transplants complications, especially the rate and severity of the corneal graft rejection.
Future treatment for keratoconus is prevention. Molecular genetics are currently being studied and we hope to identify people who are predisposing for the condition in an attempt to discover early and apply preventive treatment.